Prevención y promoción de la salud
Este es un documento vivo (más información) titulado "Prevención y promoción de la Salud" y desarrollado en el espacio del equipo Web de trabajo colaborativo en prevención y promoción de la salud.
Se ha incluido como capítulo 3 en el libro sobre polipatología (índice y PDF del libro; PDF del capítulo en inglés, PDF del capítulo en español).
Puede seguir todos los comentarios aquí o suscribirse a su canal RSS.
Para cualquier comentario, duda, sugerencia o si necesita soporte técnico, por favor no dude en contactar con nosotros en info@opimec.org
A continuación, ¡DISFRUTE del contenido del documento y PARTICIPE en mejorar el conocimiento sobre la polipatología!
Tabla de contenidos
- Viñeta: ¿Cómo podría ser?
- Resumen
- ¿Por qué es importante este tema?
- ¿Que sabemos?
- Prevención primordial y primaria
- Factores sociales determinantes de las enfermedades crónicas
- Consumo de tabaco
- Dieta y Actividad Física
- Prevención primaria: ¿Tratar a grupos de población o a pacientes individuales?
- La poli píldora
- Prevención secundaria
- Juntar todas las piezas
- ¿Qué hay que saber?
- General
- Prevención primordial y primaria
- Prevención secundaria
- ¿Qué estrategias innovadoras podrían acortar las distancias?
- Contribuyentes
- Referencias (pulse aquí para acceder)
- Licencia Creative Commons
Use el botón “pantalla completa” ![]() para aumentar el tamaño de la ventana y poder editar con mayor comodidad.
para aumentar el tamaño de la ventana y poder editar con mayor comodidad.
En la esquina superior izquierda elija el formato del texto seleccionando en el menú desplegable:
- Párrafo: para texto normal
-Capítulo de primer nivel, de segundo, de tercero: para resaltar los títulos de las secciones y construir el índice. Aquellos enunciados que resalte con este formato aparecerán automáticamente en el índice del documento (tabla de contenidos).
Use las opciones Ctrl V o CMD V para pegar y Ctrl C/CMD C para copiar, Ctrl X/CMD X para cortar (en algunos navegadores no funcionan los botones habilitados para ello)
Al finalizar la edición no olvide guardar los cambios pulsando el botón inferior izquierdo Guardar o Cancelar si no quiere guardar los cambios efectuados
Más información aquí
Viñeta: ¿Cómo podría ser?
Estamos en el año 2020. Carlos tiene 85 años. Tiene diabetes y enfermedad cardiaca, pero se las arregla para vivir bastante bien solo con el apoyo de la tecnología. Cuando era más joven, había poco interés en la prevención en su comunidad. Carlos fumaba, seguía una dieta poco saludable y no hizo mucho ejercicio durante la adolescencia y la juventud. Sin embargo, en los últimos quince años, Carlos ha puesto mucho más interés en la prevención, en continuar con el desarrollo de un entorno de fomento de la salud en su comunidad y en su país.
El Dorado, la comunidad donde vive Carlos, ha cambiado muchísimo durante los últimos 35 años. Se ha convertido en un lugar mucho más sano para vivir. En muchas tiendas se vendía comida preparada y comida rápida, pero ahora, en cambio, es más fácil comprar frutas y verduras frescas. Del mismo modo, las tiendas del barrio solían vender tabaco, y los bares y cafeterías estaban llenas de humo. Hoy en día, todos los lugares públicos son libres de humo y es poco habitual ver a una persona fumando. Hacer ejercicio era difícil en el pasado, ya que las calles estaban llenas de tráfico. Ahora, sin embargo, la densidad del tráfico ha disminuido y ha aumentado el número de personas que van en bicicleta. De hecho, el propio Carlos iba en bici hasta hace cinco años.
A nivel nacional, el gobierno también ha trabajado duro para desarrollar políticas que puedan reducir las desigualdades sociales y sanitarias en esta zona. Estas desigualdades eran una de las razones principales por las que las personas de su país sufrían múltiples enfermedades crónicas (por ejemplo, viviendas en malas condiciones, aire, comida y agua de poca calidad, y niños que no habían empezado su vida de forma saludable).
A partir de los sesenta años, Carlos se sometía regularmente a un examen médico por el riesgo de sufrir enfermedad cardiaca e infarto, aneurisma aórtico abdominal (dilatación de la arteria principal que sale del corazón), cáncer de intestino, retinopatía diabética y presión sanguínea alta. Los resultados del reconocimiento indicaron que tenía un riesgo alto de enfermedad cardiaca y de infarto y, a la edad de cincuenta años, además de mejorar su comportamiento respecto a la salud, empezó a tomar una polipíldora (una pastilla que contiene medicamentos que disminuyen la presión sanguínea y los lípidos en la sangre, y la probabilidad de la formación de coágulos en la sangre).
Los servicios sanitarios de su localidad también se han orientado mucho más hacia la atención a pacientes con múltiples problemas de salud. A partir de los sesenta años, un trabajador sanitario de la comunidad se ponía regularmente en contacto con Carlos. A partir de los setenta, le visitaba una enfermera, que acudía con más frecuencia si Carlos tenía problemas. Desde entonces, los avances producidos en la tecnología le han permitido enviar regularmente informes acerca de las diferentes pruebas médicas que se ha autorealizado, y una enfermera se ha puesto en contacto con él cuando ha sido necesario. También cuenta con un trabajador sanitario de la comunidad que va a menudo a su casa para ofrecerle apoyo emocional y social, para ayudarle y para que esté animado y no pierda la esperanza. La combinación de la enfermera, el trabajador sanitario de la comunidad y la tecnología, utilizados de forma coordinada, le ha permitido estar en casa, a pesar de tener muchas limitaciones en las cosas que puede hacer. La familia de Carlos le ayuda a gestionar su salud y tiene el apoyo del sistema sanitario y de atención social para asegurarse de que está tan sano como sea posible.
Crear las condiciones que han ayudado a Carlos a estar sano, a pesar de sus limitaciones, y a vivir en casa, ha dependido, en gran medida, de la construcción de una cultura de la salud en su comunidad y de los esfuerzos de los planificadores, las autoridades locales y los gestores de servicios sanitarios. Muchos de los servicios a los que tiene derecho se ofrecen de forma rentable; esto se consigue asegurándose de que los profesionales de la salud utilizan sus habilidades prácticas al completo y de que la atención se coordina, y ofreciendo la combinación adecuada de capacidades que se necesitan para obtener unos resultados óptimos de salud.
Resumen
- Es importante entender la trayectoria de salud y las condiciones de vida que provocan comorbilidad y enfermedades crónicas múltiples con el fin de determinar cuáles son los enfoques más eficaces de la prevención para tratar a los pacientes individuales y a los grupos de población.
- La prevención se puede clasificar en los siguientes cuatro tipos, que pueden aportar un marco útil de reflexión acerca de la prevención y la polipatología: prevención primordial, primaria, secundaria y terciaria.
- Hay tres factores de riesgo evitables que contribuyen en gran medida a una enfermedad crónica: el consumo de tabaco, una dieta poco saludable y la falta de actividad física. Es necesario analizar estos factores de riesgo en todos los niveles de la sociedad, desde los gobiernos a las personas individuales, prestando una atención especial a los grupos de población que tienen el mayor riesgo de desarrollar una enfermedad crónica.
- Se debería animar a todas las personas, con el apoyo de su comunidad, a dejar de fumar, seguir una dieta sana y practicar ejercicio regularmente. En algunos casos, es posible que se pueda hablar de un nivel de riesgo que justifique un tratamiento farmacológico.
- Existe una estrategia radical y polémica para prevenir los ataques al corazón y los infartos, que consiste en que cualquier persona mayor de 55 años empiece a tomar una pastilla que combine medicamentos que hagan bajar la presión sanguínea y los lípidos en la sangre, así como la probabilidad de que se produzcan coágulos en la sangre (conocida como polipíldora).
- Realizar reconocimientos preventivos a grupos de población con el fin de detectar los primeros signos de una enfermedad puede tener un papel importante en la prevención, pero es importante que se cumplan una serie de criterios, entre los que se encuentran la utilización de una prueba fiable, un tratamiento eficaz, la posibilidad de detección precoz de una patología mucho antes de que se manifieste una enfermedad grave por sí misma, y la rentabilidad.
- Cada vez se usan más directrices para gestionar a pacientes que sufren enfermedades crónicas, pero normalmente están pensadas para tratar a pacientes con una sola enfermedad. Combinar las directrices pensadas para pacientes con una sola enfermedad para tratar a pacientes con múltiples enfermedades puede que no solo sea ineficaz, sino que podría ser incluso peligroso.
- Se ha demostrado de forma concluyente que las tecnologías de la información y la comunicación, y en especial, las que fomentan la telesupervisión y la teleconsulta, mejoran los resultados para pacientes con enfermedades crónicas y disminuyen los costes, principalmente, porque hacen que disminuya el número de ingresos en los hospitales.
¿Por qué es importante este tema?
Está claro que cuando los pacientes con enfermedades crónicas complejas son tan habituales y sufren tantas complicaciones e ingresos no adecuados en el hospital, la prevención y el fomento de la salud son importantes.
Sin embargo, en el contexto de la polipatología, la prevención debería centrarse en crear las condiciones para evitar que los pacientes desarrollaran otros trastornos y evitar que se presentaran complicaciones de las patologías existentes. Muchos de estos pacientes serán mayores y se encontrarán al final de sus vidas, y tendrán al mismo tiempo problemas psicológicos y sociales. De hecho, puede que sus preocupaciones personales, familiares y sociales tengan poco que ver con las enfermedades que padezcan, y es esencial que el cuidado preventivo se centre en la persona, no en la enfermedad. Por ejemplo, puede no ser adecuado presionar para conseguir que un paciente deje de fumar, como sería en el caso de una persona joven, si para el paciente mayor el hecho de fumar representa algo muy importante.
Los legisladores estarán muy interesados en la prevención y en la polipatología, ya que una pequeña reducción del porcentaje de ingresos en los hospitales y en las tasas de complicación puede suponer un ahorro considerable, aspecto que es importante para el sistema sanitario en conjunto. Todos los grupos implicados deberían estar interesados en la prevención y en el fomento de la salud en relación con la polipatología, porque sabemos muchas cosas acerca de la prevención de enfermedades crónicas individuales, pero poco acerca de la prevención y del fomento de la salud entre personas que padecen múltiples enfermedades crónicas. Sin embargo, como hemos descrito anteriormente, estos pacientes representan una parte muy importante del trabajo y de los costes dentro del sistema sanitario.
¿Que sabemos?
A pesar de las páginas que ocupa este capítulo, hay muy pocos datos acerca de cuál es la mejor manera de aplicar la prevención de la polipatología, ya que todavía nos encontramos en una fase en la que estamos empezando a comprender a esta población y los factores determinantes que influyen en ella.
Una forma útil de plantearse la prevención es dividirla en prevención primordial, primaria, secundaria y terciaria, y considerar estos diferentes niveles en el contexto de las enfermedades crónicas complejas. Las siguientes definiciones de estos términos se han extraído del libro de la OMS sobre epidemiología básica (1).
La prevención primordial se ocupa de crear las condiciones económicas, medioambientales y sociales que favorecen la salud y que minimizan la probabilidad de desarrollar una enfermedad. Un ejemplo de esto podría ser reducir la pobreza. Las enfermedades cardiacas y los infartos suelen ser más frecuentes entre las personas pobres.
La prevención primaria se centra en los factores causales específicos, como el consumo de tabaco, una dieta poco sana y la falta de actividad física, en el caso de las enfermedades crónicas, con el fin de reducir las probabilidades de que la gente desarrolle una enfermedad. Como ejemplos de este tipo de prevención podemos mencionar subir los impuestos para reducir el consumo de tabaco y ofrecer programas para dejar de fumar. Otro ejemplo podrían ser las políticas orientadas a reducir el contenido en sal de la comida preparada.
La prevención secundaria se ocupa de identificar a las personas que tienen una enfermedad establecida pero que, normalmente, está en una fase temprana, para limitar la exacerbación de la enfermedad y el desarrollo de complicaciones. Un ejemplo de esto podría ser tratar a los pacientes diabéticos para controlar el nivel de azúcar en la sangre y la hipertensión, con el fin de minimizar y retrasar este tipo de complicaciones.
La prevención terciaria se centra en los pacientes con una enfermedad bien establecida y tiene como objetivo minimizar el sufrimiento y las complicaciones. La prevención terciaria es similar al tratamiento y la rehabilitación y quizá es directamente más importante para pacientes con una enfermedad crónica compleja. Un ejemplo de prevención terciaria sería un programa de gestión de una enfermedad, en el que los gestores del caso hacen el seguimiento de los pacientes, puede que por teléfono, y les motivan para que sigan tratamientos preventivos y se presenten para realizarse pruebas de reconocimiento preventivo.
Dividir la prevención en estas categorías no es más que una manera de reflexionar acerca de la polipatología y los diferentes niveles que a menudo se entremezclan y se solapan. Los australianos tienen una frase: “planeta sano, lugares sanos, gente sana”, que expresa cómo se solapan estos niveles (2). A las personas les resulta muy difícil estar sanas si viven en lugares poco sanos en los que, por ejemplo, el agua y el aire están contaminados, es habitual que se fume, se tiene a mano comida con un alto contenido en grasas y en sal en lugar de frutas y verduras, y donde es difícil encontrar un lugar para hacer ejercicio. Además, a medida que todo el planeta se vuelve menos sano debido al cambio climático, la contaminación y la urbanización, también es cada vez más difícil crear lugares sanos.
En este capítulo se hablará de todas las categorías de prevención, excepto de la prevención terciaria, que se abordará en el capítulo 6.
Prevención primordial y primaria
Factores sociales determinantes de las enfermedades crónicas
Las circunstancias sociales, medioambientales y económicas en que se desarrolla la vida de las personas son básicas para determinar su salud y las probabilidades de desarrollar una enfermedad crónica. La esperanza de vida varía hasta en cuarenta años entre los distintos países y en más de diez años dentro de un mismo país. Los ingresos, la educación, la vivienda, el empleo, las redes sociales y muchos otros factores influyen y están interrelacionados, como ha reconocido la OMS en su informe decisivo acerca de los factores sociales determinantes de la salud. (2a) El acceso a la atención sanitaria también es un factor social determinante de la salud. Cualquier estrategia ideada para reducir las enfermedades crónicas debe reconocer la importancia de estos factores sociales determinantes, y las estrategias que no los tengan en cuenta solo conseguirán tener un impacto limitado.
Las enfermedades crónicas tienen tres causas evitables principales: el consumo de tabaco, una dieta poco sana (que incluye el consumo excesivo de alcohol) y la falta de actividad física. El debate que planteamos a continuación es una presentación de lo que sabemos acerca de reducir el consumo de tabaco y fomentar la comida sana y la actividad física.
Consumo de tabaco
El consumo de tabaco mata a cinco millones de personas cada año en total, y puede que esa cifra aumente hasta diez millones para 2030 (4). La mitad de los fumadores muere prematuramente a consecuencia del tabaco y, sin embargo, si las personas dejan de fumar, pueden volver a tener el mismo riesgo que los no fumadores una vez transcurridos de diez a quince años.
En todo el mundo se ha reconocido el gran peligro que representa el tabaco y, en consecuencia, la OMS, por ejemplo, ha creado la Convención Marco para el Control del Tabaco, que obliga a los países a regular las ventas de tabaco, reducir la demanda de tabaco por parte de los consumidores, mejorar el medio ambiente y la salud de los trabajadores del sector tabaquero y fomentar la investigación. Un total de 168 países de los 192 posibles han firmado la Convención; Estados Unidos e Indonesia son los países más grandes que no han seguido el ejemplo.
Sabemos mucho acerca de las medidas de salud pública que resultan eficaces para reducir el consumo de tabaco. La OMS ha recopilado el paquete MPOWER (acrónimo que corresponde a las iniciales de las políticas en inglés), que recoge seis políticas que se sabe que funcionan (4).
Se trata de lo siguiente:
- Supervisar el consumo de tabaco y las políticas de prevención
- Proteger a las personas del humo del tabaco
- Ofrecer ayuda para dejar de consumir tabaco
- Avisar acerca de los peligros del tabaco
- Hacer respetar las prohibiciones referentes a la publicidad, la promoción y el patrocinio del tabaco
- Subir los impuestos del tabaco.
Es necesario apoyar la investigación en una serie de ámbitos: el control del tabaco, encuestas de los niveles de consumo de tabaco, el consumo global de cigarrillos, los efectos económicos en cada país (el tabaco conlleva pérdidas, no ganancias, ya que los costes de los daños causados sobrepasan los ingresos obtenidos a través de los impuestos), el coste del tabaco para los empresarios, los costes económicos de los incendios y de la basura generada, los costes para los fumadores, los documentos de las empresas tabaqueras, los litigios, la industria tabaquera y la contratación de científicos para la causa de las compañías tabaqueras.
Prohibir fumar en los lugares de trabajo y en los lugares públicos y aumentar los impuestos que gravan el tabaco son dos de las intervenciones más eficaces (4).
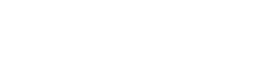
Figura 1—Eficacia de diferentes formas de terapia sustitutiva con nicotina a la hora de ayudar a las personas a dejar de fumar
La figura 1 muestra datos extraídos de la revisión Cochrane sobre las tasas de personas que dejan de fumar tras probar varias formas de terapia sustitutiva con nicotina (4,5). La gran mayoría (entre dos tercios y tres cuartos) de ex-fumadores dejan de fumar completamente sin ayuda (6,7). Este dato proviene de países que cuentan con una experiencia de veinte años fomentando de forma importante las terapias sustitutivas con nicotina, que utilizan presupuestos que hacen parecer pequeño el gasto de las campañas públicas para dejar de fumar.
La mayoría de fumadores (de largo) dejan el tabaco tras estar expuestos a políticas y campañas de alcance general y al cambio cultural respecto al tabaco. No utilizan medicamentos, ni asisten a terapia ni recurren a líneas telefónicas para ayudar a dejar de fumar. Este es un mensaje importante y muy positivo.
Casi todos los ensayos de terapia sustitutiva con nicotina se han realizado en países ricos. Estos países se diferencian considerablemente de los países de renta baja y media en lo que se refiere a su cultura de control del tabaco (fumar está mucho mejor visto en la mayoría de países de rentas bajas y medias; en la mayoría de ellos, el control sobre el tabaco es escaso, y se realizan pocas campañas para motivar a la gente a dejar de fumar). No es aconsejable esperar un interés similar en las terapias sustitutivas con nicotina por parte de la población en los países en los que la mayoría de fumadores de hoy en día están vivos.
Los países que han impuesto prohibiciones generales a la publicidad (entendiéndose prohibiciones en la publicidad en los medios y en los puntos de venta) han sido testigos de una disminución mucho mayor del consumo de tabaco que los países que no han introducido este tipo de prohibiciones (4,8). Claramente hay varios aspectos a tener en cuenta en cuanto a la causalidad en este caso, pero las pruebas que demuestran la eficacia de las prohibiciones generales son significativas. Reducir los impuestos sobre el tabaco hace aumentar el consumo, y subir los impuestos, lo reduce (4,9). Esta sensibilidad hacia el precio se ha comprobado de forma repetida en muchos países en diferentes momentos, y está bien consolidada.
Muchos de los datos acerca de reducir el daño que provoca el tabaco se centran en los cigarrillos, pero en muchas regiones del mundo, como por ejemplo el sur de Asia, son habituales otras formas de tabaco fumado, como los bidis y el tabaco oral que no produce humo, especialmente entre las mujeres y los jóvenes.
Algo de lo que sabemos mucho menos es el efecto de estas políticas, incluida la terapia sustitutiva con nicotina, en pacientes con enfermedades crónicas complejas. De hecho, de unas cuarenta revisiones Cochrane acerca de dejar de fumar, ninguna se refería a pacientes que tuvieran una enfermedad crónica establecida. Es habitual que todo un conjunto de ensayos excluyan las polipatologías o mantengan un control sobre ellas.
También es importante reconocer que el control del consumo de tabaco resulta mucho más difícil por la presencia de una poderosa industria tabaquera cuyo objetivo es promover las ventas de tabaco en todo el mundo. Estas empresas cada vez concentran más sus energías en los países de rentas bajas y medias, donde el número de fumadores y de fumadores potenciales es significativo y los controles pueden no ser muy estrictos. Estos países dependen a menudo del tabaco para su desarrollo económico.
Dieta y Actividad Física
El objetivo de reducir el tabaco está muy claro: reducir su consumo tanto como sea posible en las personas individuales y en los grupos de población, y crear, idealmente, un mundo libre de humo. Respecto a la dieta y a la actividad física, el objetivo está menos claro y continúa existiendo un intenso debate acerca de lo que se debería recomendar en ambos casos; lo mismo se aplica a decidir qué acciones generarán el mayor beneficio, para quienes y en qué condiciones.
La OMS recomienda estas directrices para las personas que deseen mejorar su dieta (10):
· Conseguir el balance energético y un peso saludable
· Limitar la ingesta de energía procedente de grasas totales y cambiar el consumo de grasas de las grasas saturadas a las insaturadas, para llegar a eliminar los ácidos grasos trans
· Aumentar el consumo de frutas y verduras, legumbres, granos enteros y frutos secos
· Limitar la ingesta de azúcares libres
· Limitar el consumo de sal de todos los orígenes y asegurarse de que la sal es yodada.
En relación con la actividad física, la OMS recomienda “como mínimo treinta minutos de actividad física regular y de intensidad moderada la mayoría de los días” (10).
Se espera que este nivel de actividad reduzca el riesgo de enfermedad cardiovascular, diabetes, cáncer de colon y cáncer de mama. Para controlar el peso es posible que se necesite más actividad. Una revisión Cochrane reciente de 43 ensayos aleatorios con 3.476 participantes descubrió que el ejercicio aumentaba la pérdida de peso en comparación con no hacer ningún tratamiento, pero que hacer régimen era más efectivo (11).
Las personas que hacían ejercicio perdieron de 0,5 a 4,0 kg, mientras que los sujetos seleccionados al azar en grupos sin tratamiento ganaron 0,7 kg o perdieron 0,1 kg. El ejercicio tenía más efecto en los factores de riesgo para la enfermedad cardiaca que en el peso, y el ejercicio más intenso provocaba una pérdida de peso mayor. Los efectos del ejercicio parecían ser diferentes en hombres y en mujeres, ya que las mujeres tenían que reducir su ingesta de calorías de forma más activa para perder peso. (12) Muchas personas con enfermedades crónicas múltiples no podrán realizar treinta minutos de ejercicio la mayoría de días, aunque, en contra de la opinión general, el Programa de Prevención de la Diabetes demostró que era más probable que las personas con sesenta años o más siguieran el consejo de hacer más ejercicio y de mejorar su dieta que los más jóvenes (13).
Aumentar la actividad física puede ser más beneficioso que mejorar la dieta en el sentido de que, además de reducir las posibilidades de desarrollar una enfermedad crónica, también mejora la calidad de vida, factor que puede ser especialmente importante para las personas que padecen una enfermedad crónica compleja (14).
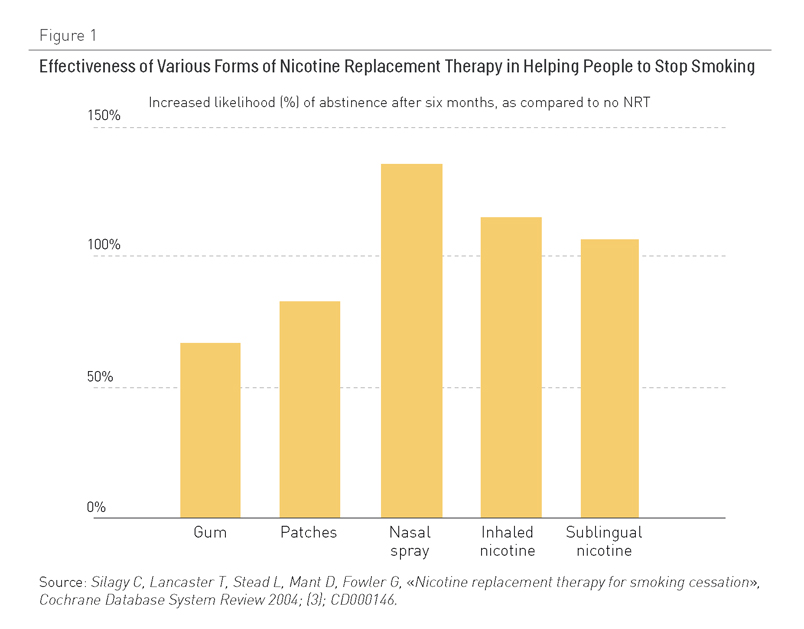
Recientemente la OMS realizó un estudio sistemático de datos que demuestran lo que funciona al aumentar la actividad física y mejorar la dieta (15). Se analizaron los datos a partir de las siguientes categorías: política y medio ambiente, medios de comunicación, contextos escolares, lugar de trabajo, comunidad, atención sanitaria primaria, adultos mayores y contextos religiosos (Tabla 1).
Tabla 1. Estudio sistemático de las intervenciones orientadas a mejorar la dieta y promover la actividad física (15)
Los revisores identificaron 395 estudios que cumplían sus criterios de inclusión, pero solo trece de ellos estaban relacionados con países de rentas medias o bajas, y solo dieciocho se ocupaban de adultos mayores. El estudio tuvo en cuenta resultados psicosociales, actitudinales y clínicos y clasificó las intervenciones como eficaces, moderadamente eficaces, prometedoras pero basadas en pocas pruebas, mínimamente eficaces, basadas en pruebas insuficientes o con eficacia no demostrada, o con resultados que no se medían o recogían en el informe. Teniendo en cuenta las limitaciones de los estudios que se incluían en el análisis, las conclusiones principales del estudio se resumen en los puntos siguientes:
- Política y medio ambiente: Se encontraron tres intervenciones que resultaban eficaces: 1) regulación gubernamental que apoye alimentos básicos más sanos; por ejemplo, sustituir el aceite de palma por aceite de soja, con lo que se reduce el contenido en ácidos grasos en la dieta; 2) políticas de construcción, planificación y transporte que disminuyan las barreras para realizar actividad física, y 3) carteles en lugares estratégicos para fomentar el uso de las escaleras. Entre las intervenciones de eficacia moderada se encuentran las políticas de fijación de precios, los carteles en los puntos de venta para animar a elegir los productos más sanos y los enfoques dirigidos a un público amplio para animar a caminar más y a ir en bicicleta.
- Medios de comunicación: Las campañas para promover la actividad física son eficaces si se combinan con programas de apoyo basados en la comunidad o relacionados con políticas para reducir las barreras medioambientales que impiden la actividad física. Entre las intervenciones de eficacia moderada se encuentran las campañas intensivas que se concentran en un solo mensaje (como aumentar el consumo de leche semidesnatada), las marcas o logotipos de salud nacionales que indican a los consumidores cuáles son los alimentos más sanos y campañas intensivas a largo plazo que promueven dietas sanas.
- Contextos escolares: Los programas escolares de alta intensidad pueden funcionar si son globales y tienen muchos componentes, entre los que se incluyen la enseñanza impartida por personas con la formación necesaria, políticas escolares de apoyo, un programa de actividad física, un componente parental/familiar y la opción de elegir comida sana en las escuelas. Los programas y evaluaciones centrados en las necesidades de las escuelas y su contexto cultural tienen una eficacia moderada.
- Lugar de trabajo: Los programas multicomponenciales para el lugar de trabajo que incluyen el ofrecimiento de comida sana y espacios para realizar ejercicio, en los que se implica al personal para su planificación e implementación, se incorporan intervenciones familiares, se ayuda a las personas a cambiar, y se cuenta con supervisión, resultan efectivos.
- Comunidad: Hay tres intervenciones que han demostrado ser eficaces en la comunidad. En primer lugar, programas de educación para la dieta con muchos componentes orientados a grupos de alto riesgo. En segundo lugar, programas de desarrollo de la comunidad que suponen la cooperación intersectorial, o tienen un único objetivo, como reducir el riesgo de un acontecimiento cardiovascular. En tercer lugar, programas basados en la comunidad para un grupo homogéneo. Varias intervenciones han demostrado tener una eficacia moderada: utilizar los servicios de consultas telefónicas para pedir consejos sobre alimentación, intervenciones comunitarias realizadas como parte de una campaña nacional o global, programas que se dirigen a la población pobre o analfabeta y que incluyen consejos sobre alimentación, intervenciones basadas en la informática que ofrecen un feedback personalizado para grupos de alto riesgo, “tours” por el supermercado para apoyar la compra de alimentos más sanos, y el autobús escolar peatonal.
- Atención primaria: Las intervenciones de atención primaria que se dirigen a personas con riesgo de padecer una enfermedad crónica pueden ser eficaces si incluyen a personas que son inactivas, que comen menos de cinco porciones de fruta o verdura cada día, que consumen muchas grasas, que tienen sobrepeso o que cuentan con una historia familiar de enfermedad crónica; si incluyen como mínimo una sesión con un profesional de la salud que negocie objetivos razonables con un seguimiento por parte de personal cualificado, y si cuentan con el apoyo de información orientada al público objetivo. Las intervenciones vinculadas con acciones que llevan a cabo otros sectores interesados, por ejemplo, instituciones deportivas o medios de comunicación, también pueden resultar eficaces. Los programas que identifican a los pacientes con altos niveles de colesterol en la sangre y ofrecen seguimiento tienen una eficacia moderada, como también la tienen los programas para perder peso que incluyen consultas telefónicas o por internet a lo largo de un periodo de cuatro semanas como mínimo y un programa de autoayuda con autocontrol.
- Adultos mayores: A pesar de que el análisis sistemático encontró dieciocho estudios de diecisiete intervenciones en adultos mayores, no identificó ninguna intervención eficaz en este grupo de edad en concreto, lo que es muy destacable para nuestro interés por las personas con múltiples enfermedades crónicas. Entre las intervenciones de eficacia moderada se encontraban las que promueven la actividad física en un contexto de grupo que utilizaban una estructura social existente o un lugar de encuentro, y las intervenciones en el hogar en las que se ofrece a los adultos mayores un acceso más fácil a frutas y verduras utilizando una infraestructura existente.
- Contextos religiosos: Las intervenciones relacionadas con la alimentación, que cuentan con muchos componentes y son adecuadas culturalmente, que se planifican y se implementan junto con líderes religiosos e incluyen sesiones de educación en grupo y estrategias de autoayuda, resultan eficaces. Las intervenciones culturalmente adecuadas orientadas a perder peso, llevar una dieta sana y aumentar la actividad física tienen una eficacia moderada.
Este estudio identifica muchas intervenciones en las que hay pruebas que demuestran que son eficaces y luego se fija en las características que al parecer comparten las intervenciones que funcionan. Estas características suelen ser: un diseño multicomponencial, adaptación al contexto local tanto cultural como medioambientalmente, uso apropiado, estructuras sociales existentes y la necesidad de la participación de los sectores interesados a lo largo del proceso.
Los autores del estudio también indican que la mayoría de estudios son a corto plazo, lo que significa que la mayoría de los resultados son más psicosociales que clínicos, y que tenernos pocos datos acerca de la sostenibilidad del programa. Pocos de esos estudios ofrecían información acerca de la rentabilidad o tenían en cuenta las consecuencias no intencionadas.
Los pocos datos de los países con rentas bajas y medias indican claramente que es importante implicar a las comunidades en todas las fases de la planificación, implementación y evaluación para lograr el éxito.
En cuanto a las polipatologías, es realmente necesario que se lleve a cabo un estudio que tenga en cuenta estos procesos y enfoques y analice su relevancia respecto a la prevención, así como la trayectoria que lleva a la polipatología. Si se contara con X prácticas o políticas, ¿se podría reducir la incidencia de las enfermedades crónicas complejas y retrasar su inicio e impacto? ¿Qué grupos de población tienen mayor riesgo de padecer una enfermedad crónica compleja? ¿Deberíamos centrarnos en grupos de población de alto riesgo en términos de política y de intervención sanitaria para la población? ¿Qué esfuerzos son necesarios para que se produzcan cambios en estos grupos de población? ¿Qué análisis se necesitan?
Un análisis exhaustivo de los barrios y la diabetes en Toronto, Canadá (ICES, 2007), ofrece información muy valiosa acerca del contexto social y físico como factor determinante de la enfermedad crónica y de quiénes tienen más riesgo, y acerca de los enfoques que pueden resultar útiles para reducir su incidencia. Esta investigación es un buen ejemplo de los nuevos enfoques del estudio de la polipatología y su prevención (16).
Prevención primaria: ¿Tratar a grupos de población o a pacientes individuales?
La prevención primordial se centra en la salud de la población; sin embargo, si pasamos a la prevención primaria, entonces se puede poner el interés en las personas y en sus familias. A la mayoría de trabajadores sanitarios de nuestra sociedad contemporánea lo que les interesa es tratar a pacientes individuales y a sus familias.
Las personas con una enfermedad establecida tienen un alto riesgo por definición, pero también se puede calcular el riesgo para las personas que no tienen una enfermedad establecida. Hay polémica en torno a cuál es la mejor manera de calcular el riesgo y a qué nivel se debe tratar a las personas. La OMS recomienda calcular el riesgo cardiovascular utilizando gráficas que combinen factores de riesgo, como la edad, ser fumador o no, o si la persona tiene o no diabetes y presión sanguínea sistólica (17). Las gráficas para países que cuentan con muchos recursos también incluyen niveles de colesterol en la sangre, pero hay gráficas que excluyen el colesterol para los lugares en los que es imposible o resulta prohibitivo acceder a los laboratorios para que midan los niveles de colesterol. Utilizar este tipo de gráficas tiene sentido porque ofrecen un cálculo del riesgo mucho más preciso que utilizando cualquier otro factor individualmente, aunque algunos expertos argumentan que la edad es un factor determinante del riesgo tan decisivo que se puede utilizar por si solo (Nick Wald, comunicación personal, pendiente de publicación).
Estas gráficas se desarrollan utilizando datos extraídos de los famosos estudios de Framingham, en Estados Unidos, donde se ha realizado el seguimiento de un importante grupo de población durante años. Algunos expertos argumentan que no es adecuado utilizar los datos de Framingham para otros países, donde la composición de la población puede ser muy diferente. El Reino Unido, por ejemplo, que probablemente tenga una población que es menos diferente de la de Framingham que muchos otros países, ha utilizado informes electrónicos para generar una nueva herramienta de valoración de riesgo llamada QRISK, que ha demostrado hacer mejores predicciones para el Reino Unido que la herramienta de Framingham (18, 19).
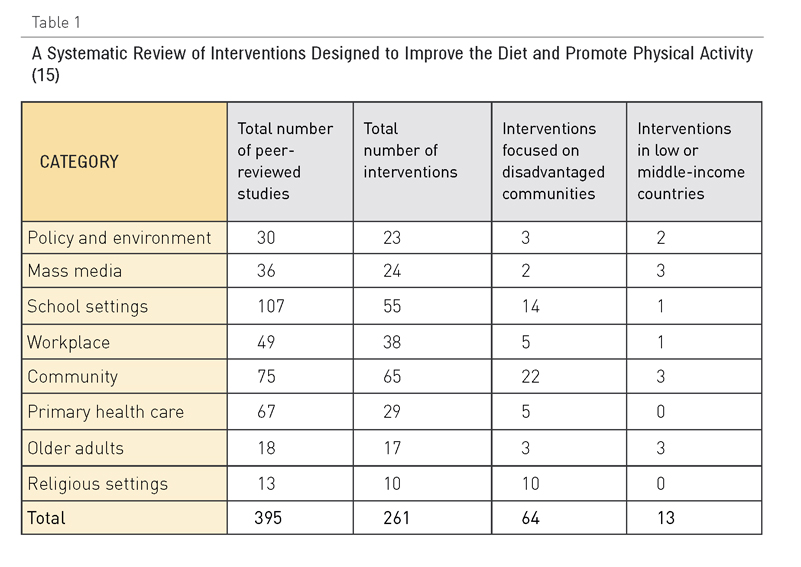
Figura 2. Superposición entre mujeres y hombres que sufrirán un acontecimiento cardiovascular en los próximos diez años a partir de las predicciones de QRISK y de las valoraciones de los riesgos de Framingham
Sin embargo, la figura 2 muestra que ninguna de las dos herramientas es demasiado buena para calcular el riesgo a nivel de la población. QRISK identifica un 10% de hombres con un “riesgo alto” (con un 20% de probabilidad de sufrir un acontecimiento cardiovascular en los próximos diez años), pero solo el 30% de los acontecimientos cardiovasculares los sufrirán esos hombres (18). En otras palabras, el 70% de los acontecimientos cardiovasculares los sufrirán hombres definidos como de bajo riesgo porque constituyen el 90% de la población. En el caso de las mujeres, es peor: QRISK identifica un 4% de mujeres de alto riesgo, pero solo el 18% de los acontecimientos cardiovasculares se dan en este grupo (19).
La OMS recomienda mejorar el estilo de vida de las personas en todos los niveles de riesgo, así como controlar regularmente a las que tienen entre un 10% y un 20% de riesgo, y someter a tratamiento farmacológico a los pacientes con un riesgo superior al 20%. El Instituto Nacional de Salud y Excelencia Clínica de Inglaterra y Gales recomienda las mismas medidas (20). La Asociación Americana del Corazón recomienda una dosis baja de aspirina para pacientes que tengan más del 10% de probabilidad de sufrir un acontecimiento cardiovascular en los próximos diez años (21). Un estudio sistemático reciente indica que puede que estos consejos sean erróneos (22).
Pero existe el argumento de que un 20% de probabilidad de sufrir un acontecimiento cardiovascular en los próximos diez años es un riesgo alto inaceptable para algo que fácilmente puede tener como consecuencia la muerte o una discapacidad grave. La gente gasta grandes cantidades de dinero cada año para asegurar sus casas, que no tienen ni de lejos una probabilidad del 20% de incendiarse o de sufrir daños graves en los próximos diez años. Por supuesto, el riesgo de un daño potencial se debe calcular contra el riesgo que conlleva el tratamiento, y por este motivo los autores del estudio sistemático reciente se muestran en contra de utilizar aspirina en personas con un riesgo bajo (22): sin duda, la aspirina reducirá las posibilidades de sufrir una trombosis que provocaría un ataque al corazón o un infarto, pero también aumenta el riesgo de una hemorragia gastrointestinal o cerebral, con lo que el riesgo del tratamiento anula cualquier posible beneficio.
La poli píldora
Con la evidencia acumulada por años, se ha buscado un tratamiento efectivo que pudiera utilizarse en individuos con cualquier nivel de riesgo para desarrollar un evento cardiovascular. El uso masivo de este tratamiento podría reducir una gran proporción de infartos del miocardio o cerebrales. El argumento en contra es que dejando de fumar, haciendo ejercicio y comiendo saludablemente se puede alcanzar el mismo efecto sin necesidad de medicación. El problema es que hasta el momento estas medidas han tenido poco efecto en la prevención de estas enfermedades.
El objetivo ha sido entonces desarrollar una sola píldora con varios fármacos que pueda ser utilizada masivamente con poco riesgo y alta efectividad como medida complementaria a los cambios conductuales necesarios para reducir el riesgo de enfermedad cardiovascular. En 2003 Nick Wald y Malcolm Law desarrollaron en una sola píldora una combinación de un anti-hipertensivo, una estatina, aspirina y ácido fólico, el cual ha mostrado, tanto en estudios clínicos como epidemiológicos, su efectividad para prevenir eventos cardiovasculares en individuos mayores de 55 años. Desde los primeros estudios publicados en BMJ en 2003 (16).
Wald y Law, así como otros autores, han mostrado que el tomar esta polipíldora puede prevenir infartos del miocardio y cerebrales con un 80% de efectividad contra un 20% de riesgos colaterales cuando se administra en forma contínua a individuos de diferentes países. Las personas de 55 años, simplemente debido a su edad, tienen un 8% de riesgo de sufrir evento mayor cardiovascular en los siguientes 10 años. Por tal motivo una dosis diaria de una estatina, aspirina, ácido fólico y tres antihipertensivos puede reducir en un 80% su riesgo de sufrir un infarto del miocardio o cerebro vascular. Estudios recientes han cuestionado el uso de la aspirina como constituyente de esta poli píldora y la versión de Wald y Law no contiene aspirina (15).
El añadir acido fólico siempre ha ocasionado controversias y otras poli-pildoras no lo incluyen. La simplicidad de la idea de Wald y Law y las pruebas de su efectividad muestran que se pueden salvar muchas vidas en individuos a riesgo utilizando un medicamento sencillo en vez de tratamientos complejos utilizando diferentes fármacos por separado.
El costo de producción de esta píldora es de menos de un dólar americano por mes ya que los ingredientes utilizados no tienen patente. Esto la hace accesible para países pobres donde sería difícil proveer a grandes sectores de la población con medicamentos utilizados en tratamientos convencionales.
Esta idea revolucionaria ha tenido gran aceptación en algunos sectores y un rechazo absoluto en otros. La idea de proveer un tratamiento de calidad inferior ha sido muy discutida entro los cardiólogos, quienes al mismo tiempo aceptan que en el futuro habrá un incremento severo de muertes por enfermedad cardiovascular en individuos que están a riesgo y no tienen acceso a servicios de salud de calidad. Al mismo tiempo, algunos profesionales de la salud pública han considerado que el uso de la polipíldora podría disminuir el uso de medidas para mejorar el estilo de vida saludable que tanto se ha tratado de buscar. Finalmente, las compañías farmacéuticas han visto en esta intervención una disminución de mercado potencial y han atacado al medicamento con el argumento de que su uso conduciría a una “medicalización” de las personas mayores de 55 años de edad.
Aunque el progreso de esta idea ha sido terriblemente lento desde el punto de vista de los entusiastas, la idea de la polipíldora esta en un momentum creciente y actualmente existen varias polipíldoras disponibles, la mayoría producidas en la India. Un estudio de factibilidad realizado en ese país ha mostrado que es posible producir una píldora con todos los componentes para reducir en forma significativa los factores de riesgo, aunque quizá no suficiente para reducir los infartos del miocardio y cerebro vasculares en un 80% de la población a riesgo (17).
Algunas personas en la India están tomando esta píldora y existe la posibilidad de que pronto esté disponible un medicamento similar para venta como prevención secundaria en el mercado europeo y norteamericano. Existe evidencia de que el uso de esta píldora puede ser efectivo para prevenir un segundo evento en personas que han sufrido un infarto del miocardio o cerebro vascular y de que muchas de estas personas no están tomando el medicamento a pesar de su indicación(18).
Al mismo tiempo, se está planeando en la actualidad un estudio para evaluar la efectividad de la polipíldora como parte de programas de prevención primaria de enfermedades cardiovasculares. Se busca que los resultados puedan contrarrestar los argumentos de aquellos que están dudosos o contrarios a su uso. Es dudoso, sin embargo, que el diseño de este estudio convenza a aquellos que argumentan que los individuos bajo tratamiento con este simple medicamento tiendan a aumentar su riesgo de enfermedad cardiovascular al sentirse “protegidos” con uso y, por lo tanto, menos predispuestos para adoptar un estilo de vida más saludable que los lleve a un mayor riesgo.
Una cuestión interesante sería si combinar varios fármacos para el manejo de individuos con enfermedad crónica compleja sería tan efectivo como en las enfermedades cardiovasculares. En este segundo caso estarían padecimientos como el tratamiento simultáneo del asma, la enfermedad pulmonar obstructiva crónica y la depresión. La polifarmacia siempre ha sido vista con malos ojos por su asociación con tratamientos irracionales y mal diseñados. Sin embargo, cuando es posible conjuntar en forma racional un grupo de fármacos ya existentes y de bajo costo en un solo medicamento que pueda hacer un tratamiento accesible a millones de individuos que los necesitan, su desarrollo puede representar una mejor solución que el uso de innumerables recursos para desarrollar nuevos medicamentos con un posible beneficio marginal.
Prevención secundaria
La prevención secundaria se centra en las personas que tienen una enfermedad establecida, aunque suele encontrarse en una etapa temprana. Tiene el fin de limitar la extensión de la enfermedad y el desarrollo de complicaciones. Para que tenga éxito tiene que haber una etapa temprana en la enfermedad que se pueda identificar y un tratamiento eficaz para prevenir su progresión.
El reconocimiento preventivo, es decir, utilizar pruebas a gran escala para identificar enfermedades en personas aparentemente sanas, es una forma de prevención secundaria. La detección precoz del cáncer cervical es un buen ejemplo de ello, ya que identifica el cáncer en una etapa temprana y la cirugía puede eliminarlo. Resulta interesante que ahora exista una vacuna contra el virus del papiloma humano, que es la causa de muchos casos de cáncer cervical, lo que significa que el cáncer cervical se puede prevenir a través de la prevención primaria, en lugar de la secundaria, aunque el uso de esta vacuna sigue creando polémica.
Puede que se haya producido un aumento sustancial en la demanda de reconocimientos preventivos para garantizar la detección precoz de ciertas enfermedades debido a la famosa frase “más vale prevenir que curar”. Sin embargo, es necesario establecer el perfil coste-beneficio de estos procedimientos a nivel de la población con el fin de establecer el coste por cada vida que se salva.
Aplicar el reconocimiento preventivo de forma racional quiere decir que se deben cumplir muchos criterios antes de que se pueda introducir el reconocimiento de forma generalizada, y esos criterios son los que se muestran en la Tabla 2. La prueba en sí debe ser sensible (servir para seleccionar correctamente a las personas que tienen la enfermedad) y específica (que sea improbable que identifique, de forma equivocada, a personas que no tengan la enfermedad como si la tuvieran). Por desgracia, muchas posibles pruebas de detección precoz tienen poca sensibilidad y especificidad, lo que quiere decir que no seleccionan a todas las personas que padecen la enfermedad (falsos negativos) e identifican como si tuvieran una enfermedad concreta a personas que no la tienen (falsos positivos).
Tabla 2. Requisitos para que un programa de reconocimiento preventivo sea eficaz
Los ensayos clínicos aleatorizados resultan muy útiles para establecer la eficacia de las pruebas de reconocimiento preventivo en cuanto a la mortalidad y la morbilidad de enfermedades concretas en grupos de población, especialmente, en situaciones en las que se ha ideado una intervención para gestionar la enfermedad a partir de los resultados de las pruebas de detección. Esos ensayos se han realizado para determinar el coste de la detección precoz del cáncer de mama y estudios sistemáticos muestran que la detección precoz reduce la mortalidad, a pesar de que se han realizado a muchas mujeres biopsias de bultos en el pecho que al final han resultado no ser malignos (26).
El coste por año de vida ajustado por la calidad (QALY, en siglas en inglés) es de alrededor de 5.000 libras esterlinas en el Reino Unido, lo que está muy por debajo del punto de corte de 20.000 a 30.000 libras que utiliza el Instituto Nacional de Salud y Excelencia Clínica para decir de qué intervenciones se debería disponer como parte del Servicio de Sanidad Nacional del Reino Unido. Un año de vida ajustado por la calidad es un año de vida ajustado por su calidad o por su valor; es una medida inventada por los economistas médicos. Un año de salud perfecta se considera equivalente a 1,0 QALY. Habría que descontar el valor de un año con enfermedades. Por ejemplo, un año en que una persona se encuentre en cama por enfermedad podría tener un valor equivalente a 0,5 QALY (26).
Para cualquier programa de detección precoz que se introduzca es vital que tenga un nivel alto de garantía de calidad. En caso contrario, puede que no se consigan los resultados deseados. Por ejemplo, durante años, en Gran Bretaña la detección del cáncer cervical no contaba con garantías de calidad. Se examinaba a las mujeres equivocadas, las muestras se recogían de forma poco fiable y no se controlaba la calidad de la interpretación de la citología. El resultado fue que, antes de que se introdujera el control de calidad, se conseguía muy poco con las pruebas de detección precoz del cáncer cervical (28).
Tabla 3. Criterios del Reino Unido para valorar la viabilidad, eficacia y adecuación de un programa de reconocimiento preventivo (actualizado en junio de 2009)
La Tabla 3 muestra los criterios utilizados en el Programa de Reconocimiento Preventivo Nacional del Reino Unido para decidir qué programas se introducen. Entre los programas de reconocimiento preventivo que cumplen con estos criterios se encuentran los de detección del aneurisma aórtico abdominal, de cáncer de mama, de intestino y cervical, de la retinopatía diabética, de la hipertensión y del riesgo vascular. La Tabla IV muestra los programas que no cumplen los requisitos, a menudo pese a la presión popular que existe para que se introduzcan en el Programa Nacional.
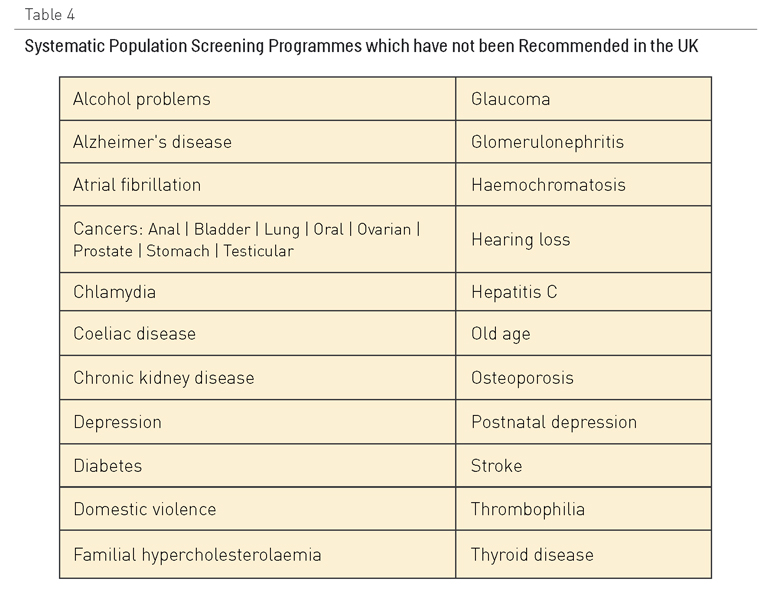
Tabla 4. Programas sistemáticos de reconocimiento preventivo para la población que no se recomiendan en el Reino Unido
Muchos grupos de población desfavorecidos, como por ejemplo, las personas con dificultades de aprendizaje o con problemas de salud mental, tienen menos probabilidades de ser sometidos a reconocimientos preventivos. Esto podría ser igualmente cierto para las personas que sufren múltiples enfermedades crónicas.
Las medidas para dejar de fumar, aumentar la actividad física y mejorar la dieta podrán ser efectivas también como estrategias de prevención secundaria en pacientes con enfermedades cardiovasculares establecidas, pero los pacientes también necesitan tratamientos farmacológicos para reducir las posibilidades de recidiva o de que surjan complicaciones en el caso de diabetes o progresión de la enfermedad respiratoria crónica. La mayoría de estos tratamientos se basan firmemente en evidencias, aunque recientemente se han hecho interesantes propuestas a partir de un ensayo importante que sugieren que mantener un control estricto del azúcar en la sangre en pacientes diabéticos puede producir peores resultados (29).
Juntar todas las piezas
A pesar de que hemos seguido la división epidemiológica clásica de los niveles de prevención, los gobiernos y las autoridades sanitarias deben decidir cuál es la combinación correcta para sus circunstancias concretas. Algunos gobiernos contarán con muy pocos recursos para los sistemas sanitarios y, por ello, se centrarán en los factores sociales determinantes de la salud. Otros gobiernos puede que operen en entornos políticos en los que cualquier forma de “ingeniería social” esté bajo sospecha y, en consecuencia, puede que se centren en estrategias orientadas a las personas enfermas.
¿Qué hay que saber?
General
- ¿Cuáles son las trayectorias de salud y las condiciones de vida que provocan comorbilidad múltiple y enfermedades crónicas complejas?
- ¿Cuáles son los enfoques de la prevención más efectivos para las personas individuales y para los grupos de población?
- ¿Cuáles son los enfoques en términos de conceptualización de la prevención en la bibliografía sobre las enfermedades crónicas que se pueden aplicar a la polipatología?
- ¿Qué es nuevo o diferente en la población polipatológica?
- ¿Qué puntos de la investigación es importante que se sigan tratando?
- ¿Cuál es la contribución relativa de la prevención primordial, primaria, secundaria y terciaria para mejorar los resultados y la satisfacción, y para reducir a la vez los costes para las personas que viven con enfermedades múltiples? ¿Cuál es la mejor estrategia de prevención que se debe seguir en cualquier tipo de circunstancias? ¿Se puede elaborar una guía que se pueda utilizar en circunstancias muy diferentes?
A continuación presentamos una lista de cuestiones políticas y de investigación para la prevención primordial, primaria y secundaria.
Prevención primordial y primaria
- ¿Cómo se podrían promover comunidades más sanas, especialmente en países de rentas medias y bajas?
- ¿Qué podría motivar a que más países, especialmente Estados Unidos e Indonesia, firmaran la Convención Marco para el Control del Tabaco?
- ¿Es posible supervisar, por países, la investigación acerca del control del tabaco, encuestas de los niveles de consumo de tabaco, el consumo global de cigarrillos, los efectos económicos en cada país (el tabaco conlleva pérdidas, no ganancias, ya que los costes de los daños causados sobrepasan los ingresos obtenidos a través de los impuestos), el coste del tabaco para los empresarios, los costes económicos de los incendios y de la basura generada, los costes para los fumadores, los documentos de las empresas tabacaleras, los litigios, la industria tabacalera y la contratación de científicos para la causa de las compañías tabaqueras?
- ¿Cuáles son los efectos de las políticas MPOWER, en especial, de la terapia sustitutiva con nicotina, en las personas que viven con múltiples enfermedades crónicas?
- ¿Cuál es la dieta y el nivel de actividad física óptimos para las personas que viven con múltiples enfermedades crónicas? ¿Hasta qué punto son sostenibles, rentables y seguras las intervenciones efectivas?
- ¿Qué políticas para mejorar la dieta y aumentar la actividad física serán efectivas en pacientes con múltiples enfermedades crónicas?
- ¿Cómo se podría motivar a las personas que viven en países de renta media y baja, que ya siguen una dieta saludable, a mantenerla en lugar de pasarse a dietas poco saludables con un alto contenido en grasas, en sal o en calorías?
- ¿Cómo se puede garantizar que, con la creciente urbanización y pobreza urbana, los habitantes de ciudades en los países de renta baja y media puedan mantener cierto nivel de actividad física?
- ¿Cuál es la mejor manera de calcular el riesgo de desarrollar una enfermedad cardiovascular, en especial en lugares en los que no se dispone de pruebas de laboratorio o es imposible permitírselas?
- ¿Se puede utilizar la edad por sí sola para valorar el riesgo? Si es así, ¿debería establecerse un nivel de corte diferente en los distintos países?
- ¿Cuál es el nivel de riesgo adecuado al que se debe iniciar un tratamiento farmacológico?
- ¿Resultará la polipíldora más rentable que el tratamiento rutinario en la prevención primaria, secundaria y terciaria?
- ¿Cuáles deberían ser los componentes de la polipíldora?
- ¿Cuál es la mejor estrategia para utilizar la polipíldora en la prevención primaria: valorar el riesgo y aplicar después un tratamiento, u ofrecer la polipíldora a todas las personas a partir de una cierta edad?
- Si la polipíldora es rentable, ¿cómo se podría conseguir que se extendiera su uso?
- ¿Podrían ser útiles otras polipíldoras en otras formas de prevención, por ejemplo, para dejar de fumar o en los casos de enfermedad pulmonar crónica?
Prevención secundaria
- ¿Podemos desarrollar pruebas de reconocimiento preventivo efectivas para las muchas enfermedades para las que no se dispone actualmente de pruebas fiables?
- ¿Es peligroso controlar estrictamente los niveles de azúcar en la sangre en pacientes con diabetes?
- ¿Los pacientes con múltiples enfermedades crónicas tienen menos probabilidad de que se les someta a pruebas de reconocimiento preventivo?
- Poner en marcha la investigación para acelerar la implementación de tecnologías eficaces.
- Los aspectos relacionados con las necesidades no cubiertas, ¿son parecidos en todos los países y grupos de población?
- ¿Las estrategias de realización de pruebas de reconocimiento preventivo deberían ser responsabilidad de una especialidad médica concreta, o no?
- ¿Podemos aprender cómo mejorar la prevención secundaria a partir de la observación directa de la estrategia del programa de tratamiento de la tuberculosis?
¿Qué estrategias innovadoras podrían acortar las distancias?
Existen dos grandes tipos de esfuerzo que podrían mejorar la atención preventiva de pacientes con múltiples enfermedades crónicas: los estudios colaborativos ideados para dar respuesta a cuestiones que quedan pendientes (véase la lista más arriba) y las intervenciones tecnológicas que tienen el fin de promover la implementación más efectiva del conocimiento del que se dispone.
Las cuestiones que quedan pendientes de respuesta en relación con la prevención de las enfermedades crónicas múltiples son tan diversas y complejas que, para responderlas, será necesario realizar grandes esfuerzos de investigación a largo plazo que trasciendan las barreras institucionales, geográficas, culturales, políticas y lingüísticas tradicionales.
Contribuyentes
Richard Smith, Cristina Rabadán-Diehl, Alejandro Cravioto y Abraham Wall-Medrano escribieron el borrador inicial de este capítulo en inglés. Alejandro Jadad aprobó el borrador antes de hacerlo público online a través de la plataforma OPIMEC, en español y en inglés. Este borrador recibió importantes colaboraciones en inglés de Simon Chapman, Katia De Pinho Campos, Murray Enkin, John Gillies, Rajeev Gupta, Yan Lijing, Beatriz Marcet Champaigne, J. Jaime Miranda, Mary Ann Sevick, Ross Upshur, y, en español, de Juan Antonio Guerra, Adolfo Rubinstein y Narcis Gusi. Richard Smith incorporó estas aportaciones a una nueva versión revisada del capítulo, que fue revisada por Renee Lyons y aprobada por Alejandro Jadad para su publicación.
Los principales colaboradores son los responsables del contenido, que no representa necesariamente el punto de vista de la Junta de Andalucía o de cualquier otra institución que haya participado en este esfuerzo conjunto.
Agradecimientos
Carlos Alvarez-Dardet y Angela Cejudo hicieron comentarios acerca del capítulo en español, y Neil Arnott, Jackie Bender, Gerald Bloomfield y Kerry Kuluski, en la versión en inglés, que no supusieron cambios en cuanto al contenido.
Cómo citar este capítulo
Smith R*, Rabadán-Diehl C, Cravioto,A*, Wall-Medrano A*, Chapman S, De Pinho K, Enkin M, Gillies J, Guerra JA, Gupta R, Gusi N, Lijing Y, Marcet B, Miranda JJ, Rubinstein A, Sevick MA, Upshur R. [*Colaboradores principales] PPrevention and health promotion. En: Jadad AR, Cabrera A, Martos F, Smith R, Lyons RF. When people live with multiple chronic diseases: a collaborative approach to an emerging global challenge. Granada: Escuela Andaluza de Salud Pública; 2010. Disponible en: http://www.opimec.org/equipos/when-people-live-with-multiple-chronic-diseases
Licencia Creative Commons