Comentarios de Prevención y promoción de la salud
Prevención secundaria
La prevención secundaria se centra en las personas que tienen una enfermedad establecida, aunque suele encontrarse en una etapa temprana. Tiene el fin de limitar la extensión de la enfermedad y el desarrollo de complicaciones. Para que tenga éxito tiene que haber una etapa temprana en la enfermedad que se pueda identificar y un tratamiento eficaz para prevenir su progresión.
El reconocimiento preventivo, es decir, utilizar pruebas a gran escala para identificar enfermedades en personas aparentemente sanas, es una forma de prevención secundaria. La detección precoz del cáncer cervical es un buen ejemplo de ello, ya que identifica el cáncer en una etapa temprana y la cirugía puede eliminarlo. Resulta interesante que ahora exista una vacuna contra el virus del papiloma humano, que es la causa de muchos casos de cáncer cervical, lo que significa que el cáncer cervical se puede prevenir a través de la prevención primaria, en lugar de la secundaria, aunque el uso de esta vacuna sigue creando polémica.
Puede que se haya producido un aumento sustancial en la demanda de reconocimientos preventivos para garantizar la detección precoz de ciertas enfermedades debido a la famosa frase “más vale prevenir que curar”. Sin embargo, es necesario establecer el perfil coste-beneficio de estos procedimientos a nivel de la población con el fin de establecer el coste por cada vida que se salva.
Aplicar el reconocimiento preventivo de forma racional quiere decir que se deben cumplir muchos criterios antes de que se pueda introducir el reconocimiento de forma generalizada, y esos criterios son los que se muestran en la Tabla 2. La prueba en sí debe ser sensible (servir para seleccionar correctamente a las personas que tienen la enfermedad) y específica (que sea improbable que identifique, de forma equivocada, a personas que no tengan la enfermedad como si la tuvieran). Por desgracia, muchas posibles pruebas de detección precoz tienen poca sensibilidad y especificidad, lo que quiere decir que no seleccionan a todas las personas que padecen la enfermedad (falsos negativos) e identifican como si tuvieran una enfermedad concreta a personas que no la tienen (falsos positivos).
Tabla 2. Requisitos para que un programa de reconocimiento preventivo sea eficaz
Los ensayos clínicos aleatorizados resultan muy útiles para establecer la eficacia de las pruebas de reconocimiento preventivo en cuanto a la mortalidad y la morbilidad de enfermedades concretas en grupos de población, especialmente, en situaciones en las que se ha ideado una intervención para gestionar la enfermedad a partir de los resultados de las pruebas de detección. Esos ensayos se han realizado para determinar el coste de la detección precoz del cáncer de mama y estudios sistemáticos muestran que la detección precoz reduce la mortalidad, a pesar de que se han realizado a muchas mujeres biopsias de bultos en el pecho que al final han resultado no ser malignos (26).
El coste por año de vida ajustado por la calidad (QALY, en siglas en inglés) es de alrededor de 5.000 libras esterlinas en el Reino Unido, lo que está muy por debajo del punto de corte de 20.000 a 30.000 libras que utiliza el Instituto Nacional de Salud y Excelencia Clínica para decir de qué intervenciones se debería disponer como parte del Servicio de Sanidad Nacional del Reino Unido. Un año de vida ajustado por la calidad es un año de vida ajustado por su calidad o por su valor; es una medida inventada por los economistas médicos. Un año de salud perfecta se considera equivalente a 1,0 QALY. Habría que descontar el valor de un año con enfermedades. Por ejemplo, un año en que una persona se encuentre en cama por enfermedad podría tener un valor equivalente a 0,5 QALY (26).
Para cualquier programa de detección precoz que se introduzca es vital que tenga un nivel alto de garantía de calidad. En caso contrario, puede que no se consigan los resultados deseados. Por ejemplo, durante años, en Gran Bretaña la detección del cáncer cervical no contaba con garantías de calidad. Se examinaba a las mujeres equivocadas, las muestras se recogían de forma poco fiable y no se controlaba la calidad de la interpretación de la citología. El resultado fue que, antes de que se introdujera el control de calidad, se conseguía muy poco con las pruebas de detección precoz del cáncer cervical (28).
Tabla 3. Criterios del Reino Unido para valorar la viabilidad, eficacia y adecuación de un programa de reconocimiento preventivo (actualizado en junio de 2009)
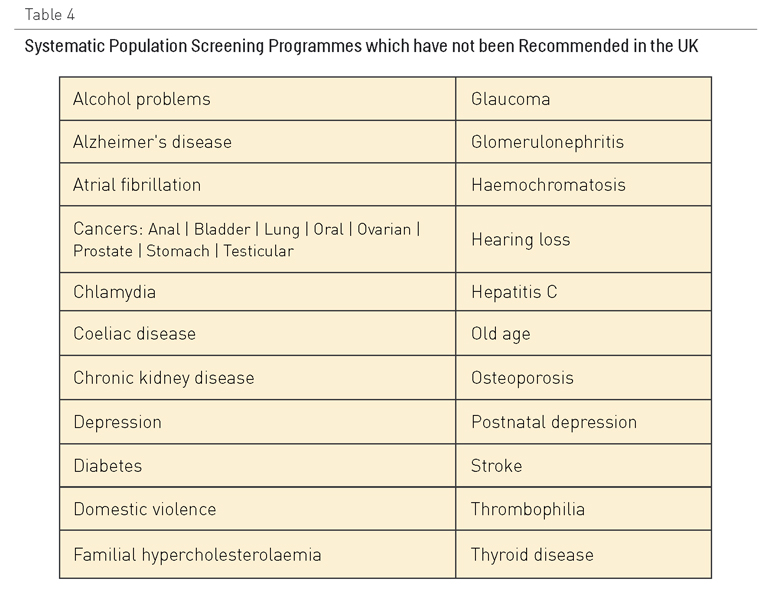
La Tabla 3 muestra los criterios utilizados en el Programa de Reconocimiento Preventivo Nacional del Reino Unido para decidir qué programas se introducen. Entre los programas de reconocimiento preventivo que cumplen con estos criterios se encuentran los de detección del aneurisma aórtico abdominal, de cáncer de mama, de intestino y cervical, de la retinopatía diabética, de la hipertensión y del riesgo vascular. La Tabla IV muestra los programas que no cumplen los requisitos, a menudo pese a la presión popular que existe para que se introduzcan en el Programa Nacional.
Tabla 4. Programas sistemáticos de reconocimiento preventivo para la población que no se recomiendan en el Reino Unido
Muchos grupos de población desfavorecidos, como por ejemplo, las personas con dificultades de aprendizaje o con problemas de salud mental, tienen menos probabilidades de ser sometidos a reconocimientos preventivos. Esto podría ser igualmente cierto para las personas que sufren múltiples enfermedades crónicas.
Las medidas para dejar de fumar, aumentar la actividad física y mejorar la dieta podrán ser efectivas también como estrategias de prevención secundaria en pacientes con enfermedades cardiovasculares establecidas, pero los pacientes también necesitan tratamientos farmacológicos para reducir las posibilidades de recidiva o de que surjan complicaciones en el caso de diabetes o progresión de la enfermedad respiratoria crónica. La mayoría de estos tratamientos se basan firmemente en evidencias, aunque recientemente se han hecho interesantes propuestas a partir de un ensayo importante que sugieren que mantener un control estricto del azúcar en la sangre en pacientes diabéticos puede producir peores resultados (29).
Comentarios existentes
Sabiendo que la prevencion secundaria es importante un aspecto, por lo menos desde Atención Primaria, es la falta de evaluación de estas medidas, las cuales no tienen un feedback back a los medicos que las realizan para conocer cual es el alcance que tienen.
Otro aspecto importante, que en algunas comunidades se esta solucionando con la historia única, es la falta de relación y comunicación entre los diferentes niveles asistenciales siendo el paciente "el mensajero" de la información y de las medidas que se han tomado.
Visto y analizando los cupos de atención primaria, tanto zonas urbanas como semiurbanas, las rurales se deberían tratar aparte, la aplicación de esta prevencion secundaria desde Atención Primaria es mayor en población mayor que en los jóvenes por lo que nos debemos plantear si se aplican a todos los pacientes.
El uso y número de pruebas diagnósticas de reconocimiento preventivo a personas aparentemente sanas se está extendiendo a medida que avanza la investigación. Muchas veces son los mismos pacientes los que se extrañan de tener que realizarse tal o cual prueba, estando aparentemente bien. El concepto de "preventivo" implica sentarse con el enfermo y/o explicarle mediante información escrita el porqué de la prueba.
Disponer de pruebas de detección sensibles y específicas, tendría un gran impacto en la identificación de personas susceptibles de desarrollar enfermedad. Una guía que dispusiera de la idoneidad de pruebas de detección como herramienta en las consultas de Atención Primaria, podría mejorar el diagnóstico de manera más temprana.
Creo que sí que es cierto que quienes son/somos diferentes podemos estar fuera del uso de estas herramientas o incluso tener una atención en la misma patología con menor intensidad
La introducción de las TIC en atención primaria a acercado los estudios complementarios a la población en general, trabajar en ese sentido seria de mucha ayuda.