Implicaciones socioeconómicas
Este es un documento vivo (más información) titulado "Repercusiones socioeconómicas" y desarrollado en el espacio del equipo Web de trabajo colaborativo en Implicaciones económicas, sociales y políticas.
Se ha incluido como capítulo 9 en el libro sobre polipatología (índice y PDF del libro; PDF del capítulo en inglés, PDF del capítulo en español).
PARTICIPE realizando comentarios a través del bocadillo que aparece en la esquina superior derecha de cada sección o bien a través de la ventana al final del documento. Si sus observaciones conducen a modificaciones sustantivas será invitada a unirse como "contribuyente" en su próxima edición.
Puede seguir todos los comentarios aquí o suscribirse a su canal RSS.
Para cualquier comentario, duda, sugerencia o si necesita soporte técnico,por favor no dude en contactar con nosotros en info@opimec.org
A continuación, ¡DISFRUTE del contenido del documento y PARTICIPE en mejorar el conocimiento sobre la polipatología!
Tabla de contenidos
- Viñeta: Como podría ser
- Resumen
- ¿Por qué es importante este tema?
- ¿Qué sabemos?
- Dependencia asociada a enfermedades crónicas
- ¿Qué hay que saber?
- Repercusiones económicas
- Repercusiones sociales y políticas
- ¿Qué estrategias podrían acortar las distancias?
- Contribuyentes
- Referencias bibliográficas (pulse aquí para acceder)
- Licencia Creative Commons
Use el botón “pantalla completa” ![]() para aumentar el tamaño de la ventana y poder editar con mayor comodidad.
para aumentar el tamaño de la ventana y poder editar con mayor comodidad.
En la esquina superior izquierda elija el formato del texto seleccionando en el menú desplegable:
- Párrafo: para texto normal
-Capítulo de primer nivel, de segundo, de tercero: para resaltar los títulos de las secciones y construir el índice. Aquellos enunciados que resalte con este formato aparecerán automáticamente en el índice del documento (tabla de contenidos).
Use las opciones Ctrl V o CMD V para pegar y Ctrl C/CMD C para copiar, Ctrl X/CMD X para cortar (en algunos navegadores no funcionan los botones habilitados para ello)
Al finalizar la edición no olvide guardar los cambios pulsando el botón inferior izquierdo Guardar o Cancelar si no quiere guardar los cambios efectuados
Más información aquí
Viñeta: Como podría ser
Laura se sintió satisfecha durante la ceremonia en la que cedía las riendas del Ministerio de Salud y Bienestar a su sucesor. Todavía no podía creer que un cambio tan grande pudiese haber tenido lugar tras sólo una década en el puesto. Como experimentada política, economista y médica de atención primaria, estaba particularmente orgullosa de exponer cómo el esfuerzo conjunto de decenas de miles de personas comprometidas de todo el país y del mundo habían dado como resultado la resolución de la mayoría de los problemas asociados a la gestión de polipatologías, que habían permanecido incorregibles durante generaciones. Podía recordar con gran satisfacción el día en el que el arriesgado y minucioso plan que ella y su equipo habían preparado había obtenido tanto el apoyo incondicional del jefe de Estado como el de legisladores, la prensa, las empresas, las organizaciones académicas y los organismos locales. Fue maravilloso ser testigo de cómo, con su apoyo, las políticas decisivas y la rápida reasignación de los recursos internos habían conducido a la puesta en marcha de un exhaustivo y generoso sistema de incentivos, que equiparaban en importancia los intereses de todos los grupos de accionistas con las necesidades sanitarias de los pacientes con múltiples enfermedades crónicas. Excediendo todas sus expectativas, había visto cómo este esfuerzo colectivo había supuesto una significativa mejora de todos los indicadores sanitarios, a un progresivo menor coste. Para ella, era particularmente satisfactorio recordar: el extraordinario apoyo prestado por otros miembros del gabinete para abordar disparidades en factores sanitarios determinantes; el entusiasmo con el que el público había promovido la ejecución de intervenciones preventivas secundarias, terciarias y cuaternarias basadas en datos; cómo toda la prensa e instituciones académicas habían puesto a la disposición de todos aquellos que lo necesitasen programas de autocuidado y educación para pacientes; cómo médicos de primera línea, gestores y cuidadores habían propuesto, desarrollado e introducido nuevos servicios sanitarios; cómo médicos con formación muy diversa habían aceptado con entusiasmo la Medicina Integral a todos los niveles; y como muchos jóvenes habían ejercido nuevas profesiones sanitarias, que ahora hacían disponibles, a todo el mundo y en cualquier sitio, servicios de atención paliativa y de apoyo. Con más del 99% de los servicios de atención sanitaria para pacientes con enfermedades crónicas múltiples siendo prestados dentro de la comunidad, su país se había convertido para otros en un faro por el que guiarse.
Laura ahora estaba preparada para embarcarse en la siguiente fase de su carrera. Había aceptado una oferta de la Organización Mundial de la Salud para dirigir una fuerza de trabajo global, que recibía el apoyo de la red existente de colaboradores y de organizaciones punteras del ámbito político, académico, médico, comunitario y empresarial, con el fin de promover la transformación de la gestión de enfermedades crónicas múltiples en todos los continentes de nuestro planeta.
Resumen
- La atención a los pacientes con enfermedades crónicas en la actualidad consume la porción más elevada del presupuesto sanitario de la mayoría de los países, con independencia de su nivel de ingresos. Se espera que esta porción global aumente de un modo significativo en las décadas venideras. La atención a pacientes con múltiples enfermedades crónicas representa el mayor consumo de recursos.
- Existe una escasez de datos sobre los impactos económicos, sociales y políticos que causan las enfermedades crónicas múltiples.
- Una integración y coordinación estrechas de los servicios sanitarios y sociales parecen determinantes para gestionar con éxito las enfermedades crónicas múltiples. Sin embargo, la mayoría de los modelos políticos, económicos y de gestión parecen seguir anclados en el pasado, debido a una excesiva compartimentación y a la falta de diálogo de las que se adolecen todos los sectores, regiones geográficas y niveles de atención.
- Dado el potencial desafío político, social y económico que presentan la gestión inadecuada de las enfermedades crónicas múltiples y el fracaso de las fuerzas de mercado para contenerlas, está justificada la intervención política, idealmente respaldada por una red global de influyentes organizaciones políticas, académicas, médicas, empresariales y comunitarias.
¿Por qué es importante este tema?
En la actualidad resulta obvio que la demanda de servicios sanitarios está saturando los recursos disponibles en todas las sociedades del mundo, lo que amenaza no sólo a la sostenibilidad del sistema sanitario, sino a la de la economía global. El aumento de la esperanza de vida es uno de los factores más estrechamente asociados a este desafío. En los EE. UU., por ejemplo, el coste sanitario de la población mayor de 85 años es seis veces mayor al de la población con edades comprendidas entre 50 y 54, y, a su vez, el doble que el correspondiente al grupo de edad comprendido entre 75 y 79 (1).
Existen diversas teorías acerca de cómo se relaciona el aumento de la esperanza de vida con la carga de la enfermedad y los costes asociados. La teoría de la expansión de la morbilidad sostiene que aumentará el número de años durante los que los humanos vivirán con enfermedades (2), mientras que la teoría de la compresión de la morbilidad (3) describe una situación en la que un aumento de años de vida saludable llevará a un aplazamiento de las enfermedades y sus costes a etapas más avanzadas de la vida (esto es, comprimiéndose en ese segmento de edad). Estas diferentes opiniones tienen importantes repercusiones sociales, políticas y económicas. Como sociedad, si invertimos en recursos para prolongar la vida de los pacientes, esto expandirá su morbilidad. Por el contrario, si establecemos los riesgos y hábitos de vida como los objetivos, probablemente retrasaremos y comprimiremos dicha morbilidad (4).
Con independencia del modo en el que las sociedades decidan asumir los desafíos asociados a las enfermedades crónicas, cualquier medida política o económica necesitará tener en consideración el hecho de que la mayoría de los costes no están asociados a los servicios clínicos sino a las pérdidas de productividad (5, 6). También se tendrá que tener en cuenta que el gasto en atención a largo plazo representará una proporción creciente de los costes de atención sanitaria en todas las economías, incluso en los modelos predictivos de contención de coste (7) más optimistas. Probablemente esto se agravará a medida que aumente el número de enfermedades crónicas que sufre una misma persona (8).
A pesar de la gravedad de la situación, ni las organizaciones ni los gobiernos están adoptando de un modo decidido medidas para luchar contra la epidemia de las enfermedades crónicas. Algunas organizaciones de consumidores sí que se están centrando en el tratamiento médico de enfermedades específicas, a veces actuando como grupos de presión para aumentar las inversiones que se realizan en tratamientos, descuidando, en cambio, la promoción de la salud y la prevención de las enfermedades. Los donantes mundiales están gastando la mayor parte de sus fondos en hacer frente a enfermedades infecciosas y en mejorar la salud materno-infantil. Por tanto, muy poco de estos fondos se dedica a luchar contra las enfermedades crónicas, y todavía menos a afrontar los desafíos asociados a la polipatología.
¿Qué sabemos?
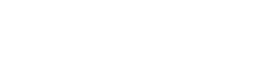
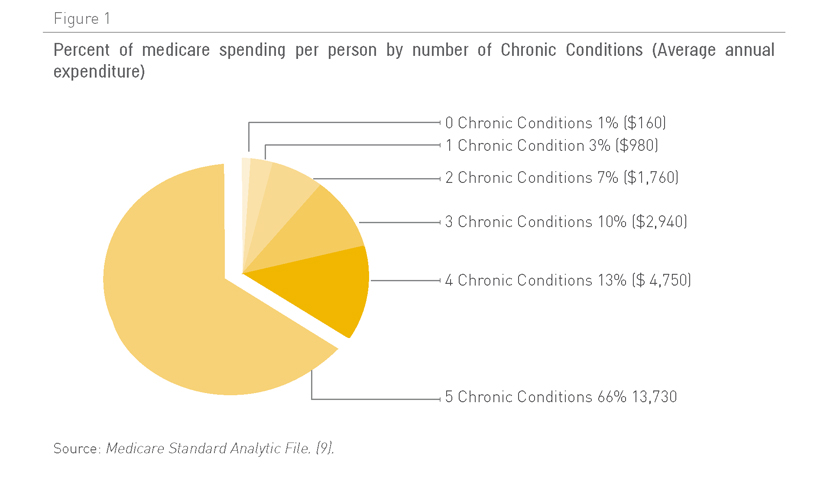
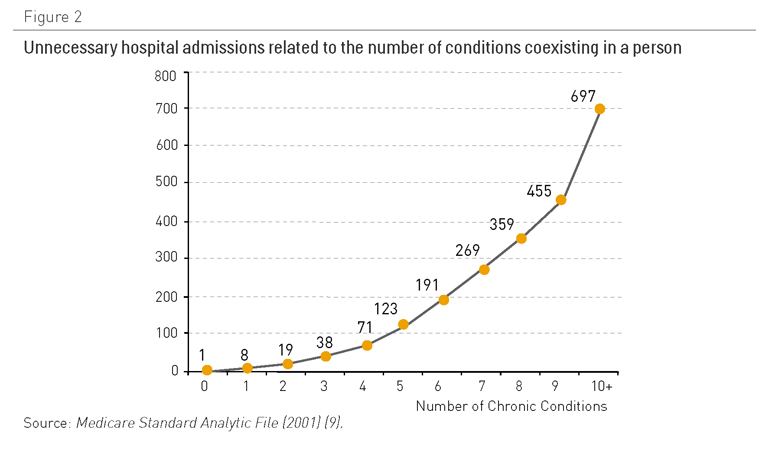
Los pacientes con cinco o más afecciones crónicas representan dos tercios del gasto de Medicare en los EE. UU. (Figura 1). No ha sido posible recabar datos similares de otros países, pero parece probable que la situación sea similar en el resto de países desarrollados. En otras palabras, la atención a los pacientes con enfermedades crónicas múltiples es cada vez más la actividad principal y supone el coste más importante para los servicios sanitarios. A medida que los pacientes padecen más afecciones crónicas, éstos tienen más posibilidades de ingresar en el hospital (Figura 2), a menudo de un modo innecesario e incurriendo en gastos considerables. En el Reino Unido, un pequeño número de pacientes, la mayoría ancianos frágiles polipatológicos, representan una gran proporción de los ingresos hospitalarios no programados (Figura 3). Estos ingresos hospitalarios entrañan un coste considerable.
Figura 1. Porcentaje del gasto per capita asumido por Medicare clasificado por número de afecciones crónicas (gasto medio anual)
Fuente: Archivo analítico estándar de Medicare (9)
Figura 2. Ingresos hospitalarios innecesarios relacionados con el número de afecciones coexistentes en una persona
Fuente: Archivo analítico estándar de Medicare (2001) (9)
Figura 3. Un pequeño porcentaje de pacientes representan muchos días de camas hospitalarias
Fuente: Análisis de encuesta entre familias británicas (2001) (10)
Existen pocos estudios disponibles sobre los costes de enfermedades crónicas para países en vías de desarrollo. Que conozcamos, tampoco hay ninguno que evalúe los costes asociados a la gestión de pacientes con múltiples enfermedades crónicas (11).
En los EE. UU. la atención a pacientes con enfermedades crónicas representa el 70% del gasto sanitario (12), pero la pérdida de productividad asociada, debido a incapacidad, bajas no programadas, descenso de eficiencia en el lugar de trabajo, el aumento de los accidentes ocupacionales o impactos negativos en la calidad del trabajo y la atención al cliente representan para los países un coste financiero todavía mayor que aquellos relacionados con los servicios sanitarios.
Figura 4. Distribución de la cobertura de Medicare y gasto en los diferentes sectores de población
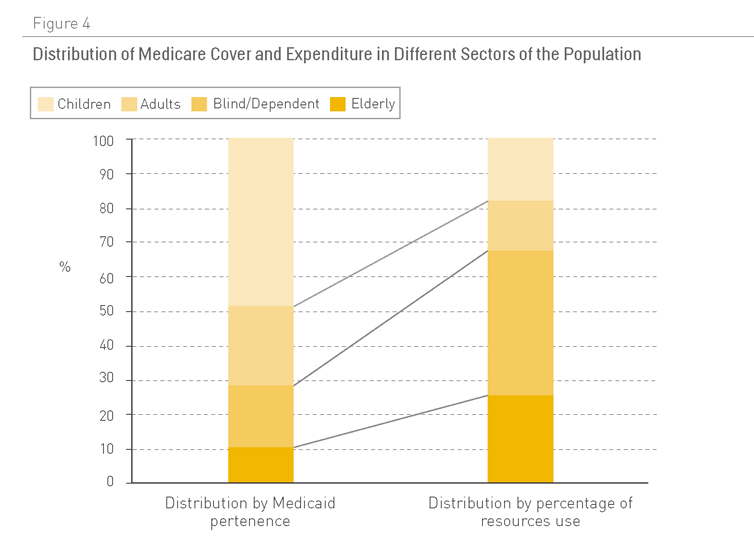
Fuente: Medicaid (13)
Dependencia asociada a enfermedades crónicas
En 2006 la OMS estimó que había 650 millones de personas con incapacidad en todo el mundo, lo que representaba el 10% de la población (14). En los EE.UU. se ha demostrado que las personas con incapacidades representan la mayor parte del presupuesto de Medicaid, a pesar de ser una minoría de casos (Figura 4) (13).
La mayoría de polipatologías están asociadas a un gran nivel de dependencia, un concepto que va más allá de la incapacidad, en tanto en cuanto implica la necesidad de apoyo por parte de una persona para realizar actividades cotidianas (como resultado de limitaciones físicas, psicológicas, intelectuales o sensoriales). Se ha estimado que los pacientes dependientes como resultado de enfermedades crónicas representan cerca del 2,5% de la población total (15).
Un reciente informe de la Organización para la Cooperación y el Desarrollo Económico (OCDE) subraya importantes niveles de disparidad entre países, en términos de cantidad de recursos disponibles para apoyar a individuos dependientes. Dicho informe también constata la falta de datos sobre la escala económica de los servicios facilitados por los cuidadores de la familia (16). Esto último supone una seria limitación para poder estimar los costes asociados a las enfermedades crónicas, a la vez que se reconoce ampliamente que son los miembros de la familia los que asumen la mayor parte de los gastos provenientes del cuidado de los pacientes dependientes (17). A medida que aumenta la proporción de pacientes dependientes y descienden las tasas de fertilidad, es razonable esperar un traspaso de esta carga y sus costes asociados de los miembros de la familia al sistema tradicional de salud y servicios sociales (18, 19).
Influencia de modos de vida y factores de riesgo de enfermedad sobre los costes sanitarios
El grado de presencia de enfermedades crónicas está estrechamente relacionado con hábitos de vida poco saludables (véase Capítulo 3). En los EE. UU., el coste estimado representado por estos hábitos en el año 2000 fue (20):
- Tabaquismo: 75,5 mil millones de dólares en costes médicos y 92 mil millones de dólares asociados a pérdidas de productividad (21).
- Obesidad y sobrepeso (2002): 132 mil millones de dólares (92 mil millones en costes directos y 40 mil millones en costes indirectos) (22).
- Mala alimentación: 33 mil millones de dólares derivados de costes médicos y 9 mil millones de dólares de pérdidas de productividad como resultado de cáncer, accidentes cerebrovasculares y diabetes, dolencias que pueden atribuirse a una mala alimentación (www.cdc.gov/nccdphp).
Un estudio descubrió que estos factores de riesgo incrementan el gasto en un 25% (23). En conjunto, tabaquismo, alcoholismo, obesidad e hipertensión consumen un 1,5% del Producto Interior Bruto en China y el 2,1% del de la India (24). Y estos costes aumentan con el incremento del número de factores de riesgo sanitario (Figura 5).
Figura 5. Coste sanitario estimado per capita en 2008 en los EE. UU. por cantidad de factores de riesgo (cifras en dólares estadounidenses)
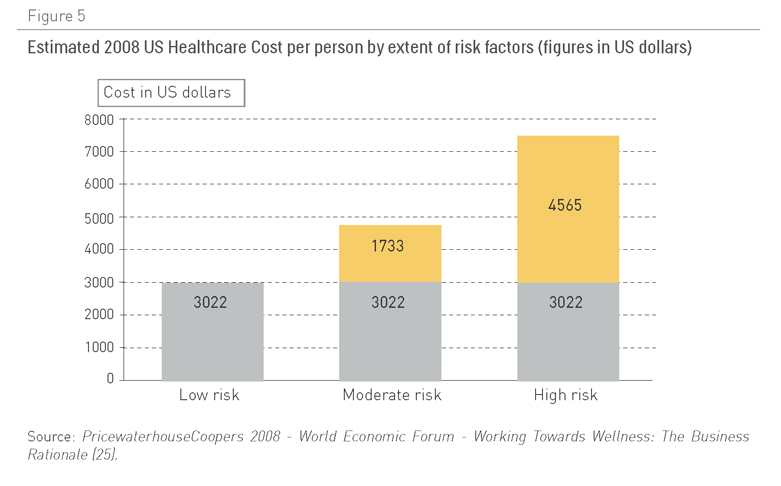
Fuente: PricewaterhouseCoopers 2008: Foro Económico Mundial: Trabajar hacia el Bienestar: la base del negocio (25)
Los costes sanitarios son más elevados en las personas sedentarias, aún sin sufrir sobrepeso, que en las personas obesas físicamente activas (26). En España, dos de cada tres niños en edad escolar y el 38% de los jóvenes adoptan conductas sedentarias en su tiempo libre (27).
Las intervenciones sobre los estilos de vida podrían tener un gran impacto en el gasto realizado en enfermedades crónicas, mediante la reducción de peso, una mejor alimentación, ejercicio regular, el abandono del tabaquismo y un diagnóstico y tratamiento temprano (Capítulo 3). Desgraciadamente, la mayoría de los países del mundo, e incluso organizaciones como la OMS, asignan recursos insuficientes para promover la salud y prevenir las enfermedades.
La OMS invirtió menos del 8% de su presupuesto en actividades relacionadas con estas dos áreas, así como con la salud mental, abuso de substancias y con la gestión de enfermedades crónicas (28). La actuación temprana sobre los factores de riesgo, ya sea con intervenciones farmacológicas o de comportamiento, tiene multitud de efectos positivos potenciales (Tabla 2).
Tabla 1. Coste por grupo de países por años de vida ajustados por calidad de medidas de control de niveles de colesterol e hipertensión
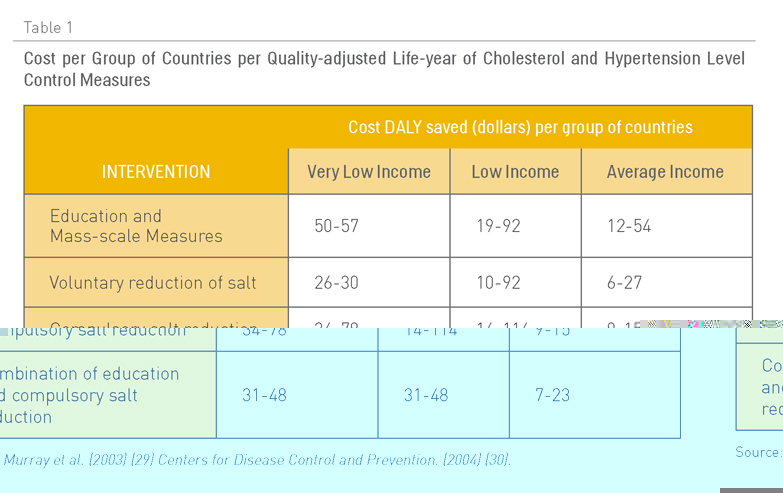
Fuente: Murray et al (2003) (29)
Centros para la prevención y el control de enfermedades (2004) (30)
¿Qué hay que saber?
La mayoría de las cuestiones relacionadas con las repercusiones económicas, sociales y políticas de las enfermedades crónicas múltiples permanecen sin ser abordadas (31).
Repercusiones económicas
- ¿Cuáles son los costes totales asociados a la gestión de enfermedades crónicas múltiples? Las estimaciones deben incluir datos sobre costes sanitarios, costes asociados a la pérdida de productividad y a la incapacidad, así como a la atención prestada por la familia para las diferentes combinaciones de enfermedades.
- ¿Cuáles son las repercusiones económicas de las diferentes estrategias para la prestación de servicios coordinados (sanitarios y sociales) para los pacientes con enfermedades crónicas múltiples?
- ¿Cuál es el modelo más apropiado de distribución de recursos de entre todas las actividades para promover la salud, prevenir enfermedades y prestar servicios sanitarios y sociales, con el fin de minimizar el impacto social y económico de las enfermedades crónicas múltiples?
- ¿Qué intervenciones podrían reducir la pérdida de productividad asociada a las enfermedades crónicas múltiples?
- ¿Qué innovaciones tecnológicas podrían ofrecer alternativas reales coste-efectivas para los modelos actuales de atención?
- ¿Cuál es el impacto de las enfermedades crónicas múltiples sobre las vidas de los cuidadores?
- ¿Qué políticas podrían conducirnos hacia una reducción del grado de presencia y consecuencias económicas de las enfermedades crónicas múltiples?
Repercusiones sociales y políticas
- ¿Cuál es el impacto de las enfermedades crónicas múltiples sobre las vidas de los cuidadores? ¿Qué nuevos papeles, flujos de trabajo y servicios de apoyo se necesitan para aliviar sus cargas?
- ¿Qué políticas podrían conducir a una reducción suficientemente importante del grado de presencia y de las consecuencias económicas de las enfermedades crónicas múltiples?
- ¿Podrían transformarse regiones clave en laboratorios vivientes con las condiciones necesarias para desarrollar, mejorar, llevar a cabo y evaluar modos innovadores de optimizar la gestión de la polipatología?
- ¿Qué estrategias se necesitan para incluir la gestión de la polipatología entre las prioridades principales para las organizaciones políticas, académicas, médicas, comunitarias y empresariales interesadas en la sostenibilidad del sistema sanitario?
¿Qué estrategias podrían acortar las distancias?
Dados los potencialmente devastadores efectos que las enfermedades crónicas múltiples podrían tener sobre la economía y sociedad en conjunto, se necesitaría desarrollar y llevar a cabo políticas decisivas para facilitar la transformación de los servicios sociales y sanitarios existentes. Tales políticas deberían, al menos, hacer más fácil la tarea de cubrir las lagunas identificadas en todos los capítulos precedentes, con una especial atención a:
- El control eficaz de la incidencia, grado de presencia e impacto de las enfermedades crónicas múltiples (Capítulos 1 y 2).
- Iniciativas audaces en la prevención de las enfermedades y promoción de la salud en todos los niveles (Capítulo 3).
- La ejecución de modelos innovadores para la gestión de enfermedades crónicas múltiples, fomentando la dirección de primera línea y la innovación vertical (Capítulo 4).
- La adaptación de los existentes servicios sanitarios y sociales para promover la óptima integración y coordinación de papeles, flujos de trabajo y procesos en todos los niveles (Capítulo 6).
- La minimización de sufrimiento innecesario y la optimización de servicios de apoyo para pacientes y sus cuidadores a lo largo de toda la evolución natural de las enfermedades crónicas múltiples, particularmente en las últimas etapas de la vida (Capítulo 7).
- Estrategias para involucrar a los pacientes con múltiples enfermedades crónicas y a sus cuidadores en programas eficaces de autocuidado (Capítulo 5), desmedicalizando así su atención en la medida de lo posible (Capítulo 8).
- Alcanzar estas metas no será tarea fácil. De hecho, podría alegarse que la lenta naturaleza del proceso de elaboración de políticas y la resistencia al cambio, que perdura en todos los niveles del sistema sanitario, interpondrán o supondrán serios obstáculos a nuestra capacidad de introducir los cambios radicales precisos para asegurar que los pacientes con enfermedades crónicas múltiples puedan alcanzar una óptima calidad de vida sin llevar la economía a la bancarrota.
Todavía no se ha tomado decisiones a este respecto. Esperemos que se tenga la previsión y el coraje necesarios para lograr: una colaboración fructífera entre el gobierno, las instituciones académicas, el público y la industria; un trabajo de investigación y desarrollo riguroso y multidisciplinario; una eficaz movilización y gestión del conocimiento, y la suficiente voluntad política para alcanzar unos desafíos sin precedentes, como consecuencia de mantenernos cada vez más con vida el tiempo suficiente para ir acumulando enfermedades crónicas múltiples.
Contribuyentes
Francisco Martos y Emilio Herrera escribieron la primera versión de este capítulo y aprobaron su traducción al inglés. Alejandro Jadad revisó la traducción al inglés detenidamente y la aprobó (con la ayuda de Francisco Martos), antes de publicarla para contribuciones externas a través de la plataforma OPIMEC en ambos idiomas. Jaime Espín aportó importantes contribuciones, y Francisco Martos las incorporó a una versión revisada del capítulo. Dicha revisión fue aprobada por Emilio Herrera y otros contribuyentes. Esta versión fue posteriormente revisada por Richard Smith. Alejandro Jadad realizó algunas modificaciones adicionales al texto y aprobó la versión final que fue incluida en el libro en soporte papel.
Agradecimientos
Narcis Gusi aportó intuitivos comentarios sobre el capítulo que no llevó a cambios en su contenido.
Cómo citar este capítulo
Martos F*, Herrera E*, Espín J, Jadad AR, Smith R. [*Principales contribuyentes] Repercusiones socioeconómicas. En: Jadad AR, Cabrera A, Martos F, Smith R, Lyons R. When people live with
multiple chronic diseases: a collaborative approach to an emerging global challenge. Granada: Escuela Andaluza de Salud Pública; 2010. Disponible en: http://www.opimec.org/equipos/when-people-live-with-multiple-chronic-diseases
Licencia Creative Commons
Repercursiones socioeconómicas por Martos F y Herrera E. está bajo licencia Creative Commons Reconocimiento-No comercial-Sin obras derivadas 3.0 España License.