Comentarios de Implicaciones socioeconómicas
¿Qué sabemos?
Los pacientes con cinco o más afecciones crónicas representan dos tercios del gasto de Medicare en los EE. UU. (Figura 1). No ha sido posible recabar datos similares de otros países, pero parece probable que la situación sea similar en el resto de países desarrollados. En otras palabras, la atención a los pacientes con enfermedades crónicas múltiples es cada vez más la actividad principal y supone el coste más importante para los servicios sanitarios. A medida que los pacientes padecen más afecciones crónicas, éstos tienen más posibilidades de ingresar en el hospital (Figura 2), a menudo de un modo innecesario e incurriendo en gastos considerables. En el Reino Unido, un pequeño número de pacientes, la mayoría ancianos frágiles polipatológicos, representan una gran proporción de los ingresos hospitalarios no programados (Figura 3). Estos ingresos hospitalarios entrañan un coste considerable.
Figura 1. Porcentaje del gasto per capita asumido por Medicare clasificado por número de afecciones crónicas (gasto medio anual)
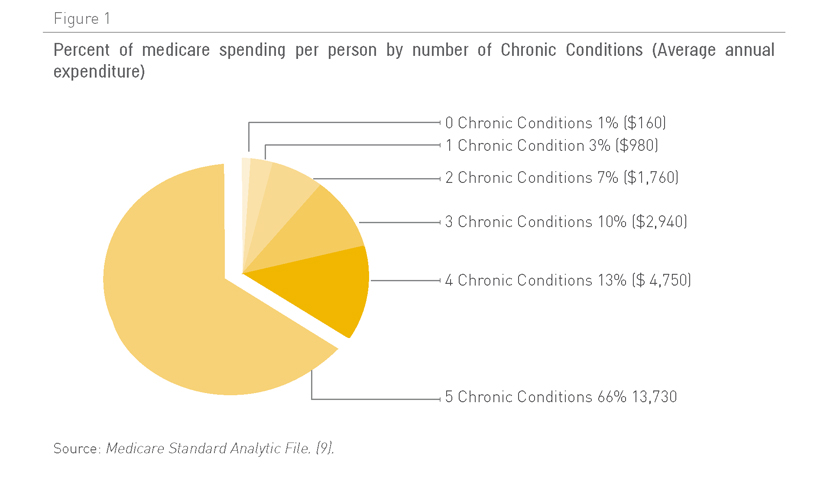
Fuente: Archivo analítico estándar de Medicare (9)
Figura 2. Ingresos hospitalarios innecesarios relacionados con el número de afecciones coexistentes en una persona
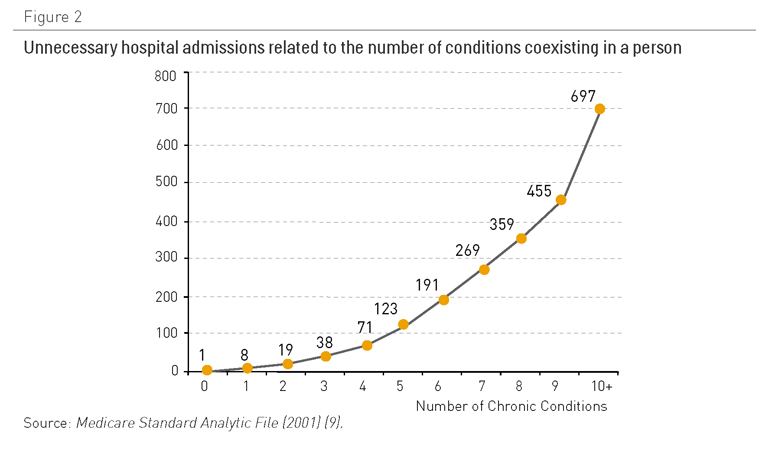
Fuente: Archivo analítico estándar de Medicare (2001) (9)
Figura 3. Un pequeño porcentaje de pacientes representan muchos días de camas hospitalarias
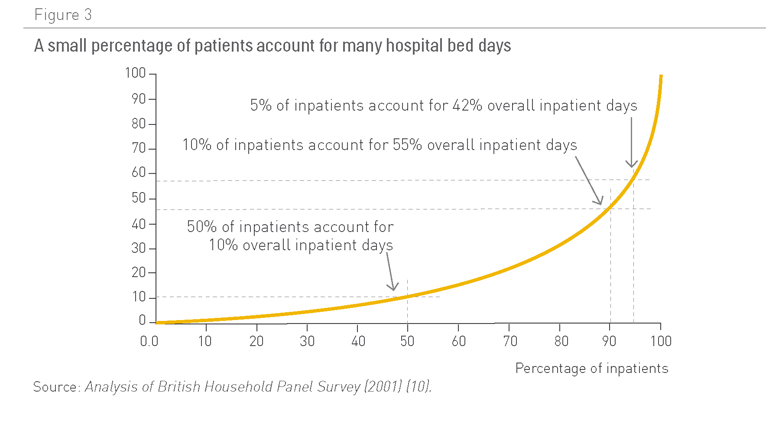
Fuente: Análisis de encuesta entre familias británicas (2001) (10)
Existen pocos estudios disponibles sobre los costes de enfermedades crónicas para países en vías de desarrollo. Que conozcamos, tampoco hay ninguno que evalúe los costes asociados a la gestión de pacientes con múltiples enfermedades crónicas (11).
En los EE. UU. la atención a pacientes con enfermedades crónicas representa el 70% del gasto sanitario (12), pero la pérdida de productividad asociada, debido a incapacidad, bajas no programadas, descenso de eficiencia en el lugar de trabajo, el aumento de los accidentes ocupacionales o impactos negativos en la calidad del trabajo y la atención al cliente representan para los países un coste financiero todavía mayor que aquellos relacionados con los servicios sanitarios.
Figura 4. Distribución de la cobertura de Medicare y gasto en los diferentes sectores de población
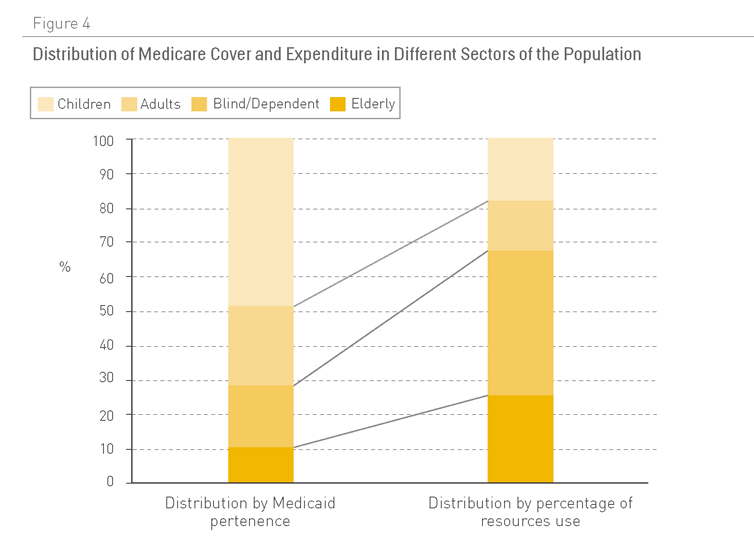
Fuente: Medicaid (13)
Dependencia asociada a enfermedades crónicas
En 2006 la OMS estimó que había 650 millones de personas con incapacidad en todo el mundo, lo que representaba el 10% de la población (14). En los EE.UU. se ha demostrado que las personas con incapacidades representan la mayor parte del presupuesto de Medicaid, a pesar de ser una minoría de casos (Figura 4) (13).
La mayoría de polipatologías están asociadas a un gran nivel de dependencia, un concepto que va más allá de la incapacidad, en tanto en cuanto implica la necesidad de apoyo por parte de una persona para realizar actividades cotidianas (como resultado de limitaciones físicas, psicológicas, intelectuales o sensoriales). Se ha estimado que los pacientes dependientes como resultado de enfermedades crónicas representan cerca del 2,5% de la población total (15).
Un reciente informe de la Organización para la Cooperación y el Desarrollo Económico (OCDE) subraya importantes niveles de disparidad entre países, en términos de cantidad de recursos disponibles para apoyar a individuos dependientes. Dicho informe también constata la falta de datos sobre la escala económica de los servicios facilitados por los cuidadores de la familia (16). Esto último supone una seria limitación para poder estimar los costes asociados a las enfermedades crónicas, a la vez que se reconoce ampliamente que son los miembros de la familia los que asumen la mayor parte de los gastos provenientes del cuidado de los pacientes dependientes (17). A medida que aumenta la proporción de pacientes dependientes y descienden las tasas de fertilidad, es razonable esperar un traspaso de esta carga y sus costes asociados de los miembros de la familia al sistema tradicional de salud y servicios sociales (18, 19).
Influencia de modos de vida y factores de riesgo de enfermedad sobre los costes sanitarios
El grado de presencia de enfermedades crónicas está estrechamente relacionado con hábitos de vida poco saludables (véase Capítulo 3). En los EE. UU., el coste estimado representado por estos hábitos en el año 2000 fue (20):
- Tabaquismo: 75,5 mil millones de dólares en costes médicos y 92 mil millones de dólares asociados a pérdidas de productividad (21).
- Obesidad y sobrepeso (2002): 132 mil millones de dólares (92 mil millones en costes directos y 40 mil millones en costes indirectos) (22).
- Mala alimentación: 33 mil millones de dólares derivados de costes médicos y 9 mil millones de dólares de pérdidas de productividad como resultado de cáncer, accidentes cerebrovasculares y diabetes, dolencias que pueden atribuirse a una mala alimentación (www.cdc.gov/nccdphp).
Un estudio descubrió que estos factores de riesgo incrementan el gasto en un 25% (23). En conjunto, tabaquismo, alcoholismo, obesidad e hipertensión consumen un 1,5% del Producto Interior Bruto en China y el 2,1% del de la India (24). Y estos costes aumentan con el incremento del número de factores de riesgo sanitario (Figura 5).
Figura 5. Coste sanitario estimado per capita en 2008 en los EE. UU. por cantidad de factores de riesgo (cifras en dólares estadounidenses)
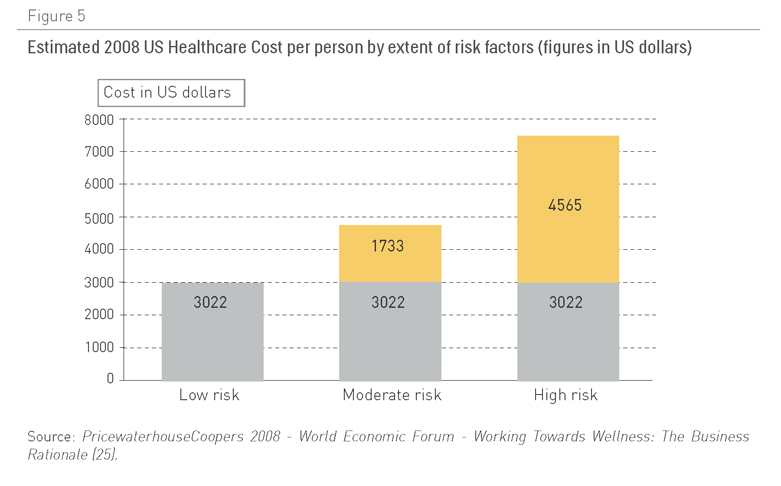
Fuente: PricewaterhouseCoopers 2008: Foro Económico Mundial: Trabajar hacia el Bienestar: la base del negocio (25)
Los costes sanitarios son más elevados en las personas sedentarias, aún sin sufrir sobrepeso, que en las personas obesas físicamente activas (26). En España, dos de cada tres niños en edad escolar y el 38% de los jóvenes adoptan conductas sedentarias en su tiempo libre (27).
Las intervenciones sobre los estilos de vida podrían tener un gran impacto en el gasto realizado en enfermedades crónicas, mediante la reducción de peso, una mejor alimentación, ejercicio regular, el abandono del tabaquismo y un diagnóstico y tratamiento temprano (Capítulo 3). Desgraciadamente, la mayoría de los países del mundo, e incluso organizaciones como la OMS, asignan recursos insuficientes para promover la salud y prevenir las enfermedades.
La OMS invirtió menos del 8% de su presupuesto en actividades relacionadas con estas dos áreas, así como con la salud mental, abuso de substancias y con la gestión de enfermedades crónicas (28). La actuación temprana sobre los factores de riesgo, ya sea con intervenciones farmacológicas o de comportamiento, tiene multitud de efectos positivos potenciales (Tabla 2).
Tabla 1. Coste por grupo de países por años de vida ajustados por calidad de medidas de control de niveles de colesterol e hipertensión
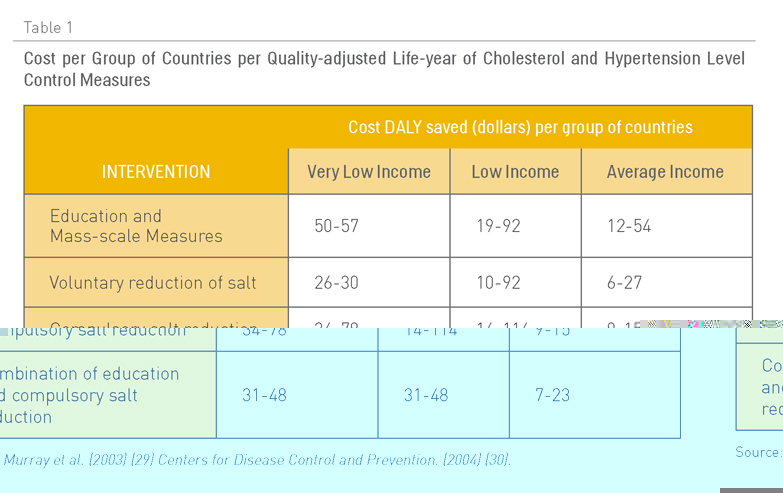
Fuente: Murray et al (2003) (29)
Centros para la prevención y el control de enfermedades (2004) (30)