Comentarios de Modelos de gestión
¿Qué estrategias innovadoras podrían acortar las distancias?
Las opiniones sobre la innovación en los modelos de gestión de enfermedades crónicas oscilan entre dos extremos, desde las predicciones más optimistas en cuanto a su impacto (78) (reducción en la mortalidad y uso de recursos, con ahorros netos al sistema), a las más escépticas, que cuestionan si merecen la pena (79).
Tal como se apunta anteriormente, hay pruebas que defienden en general la eficiencia y eficacia de las intervenciones individuales (80-87), pero todavía hay una falta de estandarización en casi todos los aspectos de estas intervenciones. Algunas prestigiosas organizaciones han propuesto el uso de una taxonomía estándar (88), y existen proyectos con el propósito de enriquecer esto centrando la atención en las enfermedades múltiples (89).
La cooperación, especialmente entre las instituciones, más allá de fronteras nacionales y culturales, resulta esencial para evitar el solapamiento de esfuerzos, para fomentar el debate público y para promover un cambio eficaz de políticas. Las nuevas tecnologías deberían desempeñar un papel importante, no sólo a la hora de facilitar encuentros y comunicaciones de larga distancia, sino también para promover el diseño y ejecución de estudios multicéntricos que usen medidas estandarizadas.
Aunque el contexto para los esfuerzos transformadores es muy favorable, introducir cambios a gran escala en los sistemas de salud para alcanzar los desafíos impuestos por las enfermedades crónicas complejas precisará planificación, cambios de gestión y esfuerzos coordinados a todos los niveles dentro del sistema sanitario.
Para conseguir cualquier cambio significativo, la política, los agentes de financiación y las direcciones de cuidado sanitario deberían tener una visión renovada del sector y entender que el campo de juego ahora implica sistemas complejos de adaptación, que han hecho que las soluciones tradicionales resulten irrelevantes. Profesionales de la salud y pacientes ya no pueden ser considerados componentes predecibles y que se pueden estandarizar dentro de un sistema impersonal.
La complejidad de este cambio deseado del sistema puede ilustrarse de un mejor modo con un ejemplo. Los estudios indican que el 76% de los reingresos hospitalarios son evitables (90) en los 30 días posteriores alta. Esto representa el 13% de los ingresos en un hospital de día moderno, una alta proporción de los cuales son pacientes crónicos complejos frecuentes (Capítulo 3).
Las pruebas indican que se podría rectificar esta situación mediante factores como: una reducción en el índice de complicaciones durante las estancias hospitalarias, la mejora de la comunicación en el proceso del alta hospitalaria, una supervisión cercana y una participación activa de pacientes en casa, así como una mejor comunicación y cooperación entre el hospital y la atención primaria después del alta. Una atención continua óptima podría hacer alcanzar estos resultados, como consecuencia de procesos de cuidado integrado que garantizan que las personas permanecen en comunicación y siguen supervisados después del alta, y que las personas encargadas de la gestión junto con profesionales sanitarrios trabajan sin fisuras a lo largo de la comunidad hospitalaria (Capítulo 6). Desgraciadamente, la mayor parte de los sistemas en todo el mundo continúan funcionando con políticas muy centralizadas y procedimientos que nutren un modelo tradicional de cuidado agudo, en el que los hospitales controlan un ecosistema fragmentado de servicios.
Con la inminente pandemia de enfermedades crónicas, y con los nuevos desafíos creados por los casos complejos, es imperativo aunar los niveles de dirección y compromiso para cambiar y abandonar el usual proceso lineal de cambio programado que domina la mayoría de sistemas (Figura 5).
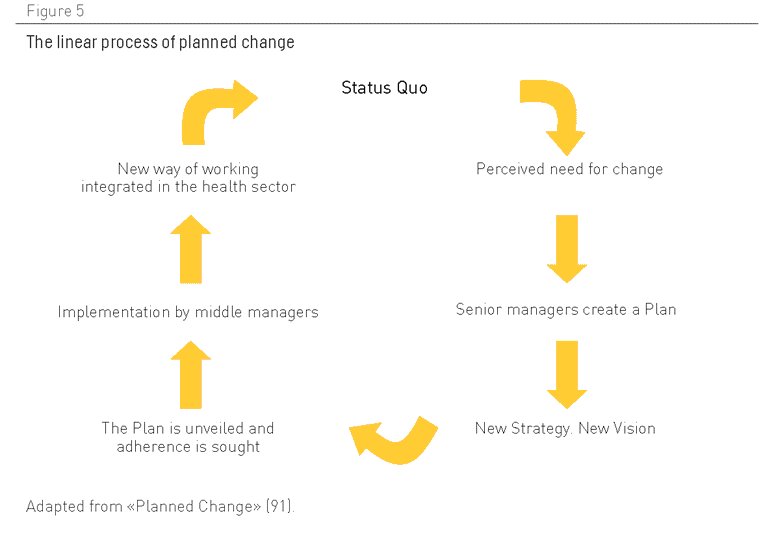
Figura 5. El proceso lineal de cambio programado. Adaptado de “Cambio Programado”(91)
Los tiempos han cambiado. Este enfoque de planificación, que cuenta con una gran presencia, refleja una visión excesivamente simplista del modo en el que las organizaciones trabajan hoy en día. Aunque se aplica con la mejor de las intenciones, con el propósito de reorganizar el sector basándose en la jerarquía y la planificación lineal descendente, este enfoque está desfasado y refleja las condiciones de una era de gestión derivada de la época industrial, con directivas centrales en una organización que define la estrategia, que crea estructuras y sistemas para influir en lo que se ha llamado “hombres de organización” (92).
Ésta es una filosofía que espera un alto grado de conformismo de sus recursos humanos, pero desde hace tiempo esto ya no se corresponde con la situación en el sector de la salud, donde el conjunto de profesionales sanitarios y de administraciones locales están crecientemente distanciados y desconectados de los aparatos de gestión y elaboración de políticas centrales del sistema.
Hoy en día, el cambio sólo será posible a través de la dirección local y la participación entusiasta de profesionales, de la administración de la salud y del público dentro del sistema de cuidado sanitario. Esto demanda también una mayor complejidad en la gestión/planificación del sistema, para permitir a profesionales y personas usuarias desempeñar un papel mucho más estratégico en el desarrollo y mejora de los modelos que se ajusten a las necesidades de pacientes con múltiples enfermedades crónicas. Esto es claramente un cambio cultural complejo para el que no existe una fórmula mágica.
Como ocurre con cualquier otro sistema complejo, se necesitarán pasos progresivos para reconstruir el sistema desde los cimientos, mientras se recurre al capital intelectual de profesionales de primera línea, administradores, pacientes y sus seres queridos. De hecho, se ha demostrado que los cambios más substanciales y sostenidos han tenido lugar en aquellas organizaciones que permiten el cambio desde abajo instigado por personas usuarias de primera línea, profesionales y la dirección (93).
Tal como se sugiere anteriormente, aquellas personas responsables de la elaboración de políticas deben dedicar mayores esfuerzos a permitir que el conjunto de trabajadores de las diversas partes de la organización (atención primaria y hospitalaria en particular) creen nuevos modos de trabajar conjuntamente y generen comunidades de práctica que estimulen el cambio organizativo. La idea es promover la iniciativa entre profesionales y la administración local, en vez de esperar que se pongan en marcha los guiones diseñados por estamentos superiores.
Esta forma más descentralizada de dirección no implica sacrificar los beneficios conseguidos en los años recientes, a través de una gestión directa y centralizada. Tampoco significa una vuelta al pasado, a un sistema en el que sus profesionales no tienen responsabilidades y no necesitan dar cuentas. En un sistema descentralizado, los que elaboran las políticas centrales y la dirección deben actuar y ser percibidos como agentes motivadores, promotores de interrelaciones a todos los niveles, que facilitan los contactos. Uno de sus papeles principales en un sistema moderno debería ser el refuerzo de incentivos para alentar a los equipos de profesionales sanitarios, administradores y miembros del público locales a experimentar con mejoras propias, facilitando la disponibilidad de recursos, analizando y comparando resultados y difundiendo las lecciones aprendidas por ellos a otros equipos dentro del sistema.
Otro papel fundamental para las personas responsables de elaborar políticas y para las direcciones centrales sería la creación de mecanismos para apoyar la formación de gestión y la promoción de dirección local. Las personas encargadas de la dirección local necesitan conocer, entre otros aspectos: cómo motivar a sus equipos, construir sistemas, involucrar a la comunidad en una gestión de cambio y armonizar las iniciativas locales con estrategias generales perseguidas por la organización global. En el País Vasco (España), por ejemplo, se ha creado una organización para cumplir este papel. Esta organización, conocida como O+Berri, tiene como una de sus funciones principales la promoción de las comunidades con las mejores prácticas dentro de la organización. A este respecto, la agencia también promueve la conectividad entre las diferentes comunidades con las mejores prácticas, a la vez que ayuda a la dirección del sector a analizar tendencias para optimizar sus estrategias, con el fin de divulgar las innovaciones y políticas a lo largo de todo el sistema.
El punto fuerte de esta forma más descentralizada de dirección y administración reside en aprovechar la capacidad intelectual del sistema y abandonar la falsa ilusión de que es posible idear un único modelo operativo para toda una región o país. Dentro de tal sistema, deberían considerarse las diferencias que existen entre las organizaciones como algo positivo, no como un inconveniente, con líderes de todos los niveles persiguiendo sin descanso nuevos modos de facilitar y permitir mejoras en los contextos que sean más receptivos a tales cambios, gracias a su esfuerzo y compromiso colectivo.
Además, necesitamos más inversiones y una búsqueda activa de nuevas ideas que se incorporen a los modelos, con formas más audaces de evaluación, que permitan una curva de aprendizaje más pronunciada (el modelo de ensayo clínico es perfecto para aislar efectos simples, pero resulta menos útil para el aprendizaje de experiencias complejas). Las nuevas formas deberían incluir la evaluación participativa que tome en consideración las perspectivas y expectativas de profesionales y personas usuarias. En contextos complejos, las técnicas de investigación cualitativas pueden abrir el camino de un modo más eficaz que las técnicas cuantitativas, que siempre estarán sujetas a subjetividades, al omitir aspectos significativos para los que no hay datos disponibles.
Lo que se necesita es un espíritu pionero para ir más allá de los modelos existentes. Quizás el cambio más radical se necesita (en el sentido de tratar con la raíz) en formas culturales de tratar con la responsabilidad de las personas en lo referente a su salud y enfermedad. Lo que falta es un compromiso claro con la capacidad de las personas de adquirir conocimiento, cambiar su conducta y permitirles escoger con libertad.
Comentarios existentes
La cooperación, sin duda, es la clave. Pero no creo que dependa tanto de los profesionales sanitarios más que de ´los gestores del sistema sanitario e incluso voluntades políticas. Y no creo, tal y como se ha dicho aqui, que suponga necesariamente más recursos.
Las políticas sanitarias, creo que han virado desde la integración de las profesiones para mejorar la práctica al mandato de lo que ahora se debe hacer. En mi opinión se han vuelto menos democráticas, cuando se alejan de la practica en aras de reducir los costes, llenan de actividades a los y las profesionales, incrementan en descontento, facilitan el desencanto en el trabajo, en definitiva se pierde calidad asistencial. Quizás sea una visisón pesimista, pero es la que por la crisis, creo vivir.
La propuesta de mejorar la práctica, y sobre todo la política que engloba tal práctica, deben de estar presentes quienes desempeñan la labor asistencial: profesionales de distintas categorías y personas afectadas de polipatologías
Creo que la respuesta la tenemos en gran medida los profesionales. Estamos tratando directamente con los problemas por ello tendríamos que ser capaces de elaborar y evaluar modelos que pudieran asegurar el cuidado integral de los sujetos con enfermedades crónicas.
La cooperación de los distintos niveles es fundamental, en un problema de la magnitud del que estamos abordando la implicación de todos desde los políticos hasta los profesionales es la única garantía de éxito.